Bridging Culture and Care: A Mobile App for Diabetes Self-Care Honoring Native American Cultural Practices
Volume 9, Issue 1, Page No 104-113, 2024
Author’s Name: Wordh Ul Hasan1, Kimia Tuz Zaman1, Shadi Alian1, Tianyi Liang1, Vikram Pandey1, Jun Kong1, Cui Tao2, Juan Li1,a)
View Affiliations
1Department of Computer Science, North Dakota State University, Fargo, 58102, USA
2School of Biomedical Informatics, University of Texas Health Science Center, Houston, 77030, USA
a)whom correspondence should be addressed. E-mail: j.li@ndsu.edu
Adv. Sci. Technol. Eng. Syst. J. 9(1), 104-113 (2024); ![]() DOI: 10.25046/aj090110
DOI: 10.25046/aj090110
Keywords: Diabetes, Self-management, Native American, Cultural Sensitivity, Participatory Design, Mobile health
Export Citations
Diabetes presents a significant public health issue for Native Americans, exacerbated by cultural nuances often ignored by conventional healthcare. To address this, we introduce a mobile app designed with the cultural context of Native American populations in mind. The app’s development followed participatory design principles, with direct input from Native American stakeholders through focus groups and interviews. The app features culturally tailored nutrition plans incorporating traditional foods, community-based support systems, and engagement with tribal health resources. An interface highlighting Native American heritage, along with gamification using cultural storytelling, aims to enhance user engagement and educational content is provided within a culturally relevant framework. This innovative integration of technology and cultural heritage in health management is anticipated to improve engagement, self-efficacy, and health outcomes for Native Americans with diabetes, serving as a blueprint for culturally sensitive health interventions.
Received: 14 November 2023, Revised: 06 January 2024, Accepted: 06 January 2024, Published Online: 26 January 2024
1. Introduction
The prevalence of diabetes among Native American (NA) populations is not only a pressing public health issue but a stark representation of existing health disparities in the United States. Data from the American Diabetes Association reveal that Native Americans endure the highest age-adjusted prevalence rates of diabetes across all racial and ethnic groups nationwide, with figures nearly twice as high as those observed in non-Hispanic whites [1]. This staggering statistic underscores the urgency for specialized healthcare approaches tailored to the distinct needs of NA communities.
One of the most pronounced obstacles in diabetes management within these populations is the limited accessibility to healthcare [2]. Geographic isolation compounds this challenge, with many NA communities situated in remote areas where healthcare facilities are sparse, under-resourced, and often miles away from those in need [3]. This situation is further complicated by socio-economic barriers such as poverty, which is prevalent in many NA communities, and lower rates of health literacy that impede the uptake and implementation of diabetes management practices [4].
Moreover, the cultural dimensions of NA life — encompassing food, lifestyle, and health beliefs — are deeply ingrained and central to their identity. However, these cultural aspects are frequently overlooked in mainstream diabetes care strategies. The resultant disconnect renders many existing diabetes management applications ineffective for NA patients, as they fail to align with the patients’ cultural contexts and lifestyle preferences [5].
Language and educational disparities between healthcare providers and NA patients can also lead to misunderstandings and misapplications of diabetes management plans, further inhibiting effective care. It is therefore imperative to embrace a diabetes management strategy that not only recognizes but integrates the cultural, socio-economic, and geographic particularities of NA patients.
Our study advocates for a diabetes self-management system that is culturally congruent with the lives and values of NA patients. This system is designed in close collaboration with the NA community, particularly engaging with members from the Lower Sioux Indian Community in Morton, MN, to gather requirements, iterate design solutions, and garner feedback on the prototype. Our methodology is inclusive, drawing upon the unique cultural traits of the NA population in our ontological framework, user interface, nutrition guidance, social networking features, and compilation of local diabetes care resources. This paper delineates the process of developing a mobile application that is not merely a tool but a culturally resonant companion for NA patients, offering tailored nutritional and lifestyle advice, fostering a strong sense of community, and enhancing the accessibility of local diabetes management resources.
By situating the lived experiences and cultural fabric of NA individuals at the forefront, we endeavor to contribute a meaningful and functional solution to the challenges posed by diabetes management in NA communities, thereby aiming to bridge the gap between healthcare availability and cultural appropriateness.
2. Related Work
The concept of cultural appropriateness in healthcare interventions is not new; it has been thoroughly investigated by numerous scholars who advocate for the integration of cultural elements to foster positive and enduring health outcomes. The consensus is clear: to be effective, health interventions must resonate culturally with the target population. Airhihenbuwa [6] posits that cultural considerations should supersede behavioral ones, suggesting that aligning health interventions with cultural norms and values is paramount. Kreuter [7] echoes this stance, highlighting the enhanced efficacy of health programs that are culturally tailored to meet the specific needs of a given group. Further expanding on this idea, Barrera [8] devised a strategic framework for the development of culturally enriched interventions, demonstrating their superiority in bolstering health outcomes in contrast with conventional approaches.
The tripartite model of culture proposed by Asad [9], which classifies culture into knowledge, practice, and change, underscores the multifaceted influence of culture on health intervention success. This model suggests that understanding cultural knowledge, respecting cultural practices, and being open to cultural change are essential for the effectiveness of health interventions. The synthesis of these scholarly insights supports the premise that embedding cultural traditions and practices within health interventions is a pivotal strategy in diminishing health disparities and enhancing the acceptability and impact of such interventions.
Despite the known benefits of cultural tailoring, there exists a conspicuous deficiency in the availability and quality of diabetes management apps that cater to culturally diverse groups. Rodríguez [10] uncovered a scarcity of diabetes management applications available in local languages and noted a lack of credible certification or scientific backing within those that are available. Brzan [11] conducted an extensive analysis of 65 mobile self-management apps for diabetes and concluded that a mere nine met the criteria to be considered comprehensive and effective for diabetes management. This finding accentuates the need for a more rigorous and patient-centric approach to app development.
Highlighting the necessity for oversight, Sneha [12] advocates for regulation, standardization, and quality control within the burgeoning market of diabetes management applications. The current landscape is marked by an influx of apps with varying degrees of reliability and efficacy, necessitating a structured framework to assure their quality. Conversely, the research conducted by Kebede [13] offers a counterpoint, illustrating the positive impact of popular diabetes management applications like mySugr, as well as continuous glucose monitoring systems, on the self-care behaviors of individuals with type 1 and type 2 diabetes.
The intersection of culture and healthcare technology is a critical focal point in enhancing the efficacy of diabetes management applications. The influence of cultural and traditional considerations on the success of such interventions is increasingly recognized in the literature. Petersen[14] underscores the profound effect of cultural practices on diabetes self-management, suggesting that these cultural influences often have a greater impact on patient behavior than the technological features of mobile applications themselves. This insight is pivotal, as it directs attention to the nuanced ways in which cultural contexts shape health-related behaviors and choices.
Echoing this sentiment, Millan-Ferro [15] advocates for the development of interventions that are culturally resonant, particularly for marginalized groups such as the Latino community in the United States. The call is for culturally sensitive tools that are not merely translations of existing resources but are built from the ground up with cultural relevance in mind. This approach ensures that interventions are more than just medically accurate—they are culturally meaningful and thus more likely to be embraced by the communities they intend to serve.
The work of Chacko [16] sheds light on the intricate ways individuals with Type 2 diabetes navigate their healthcare options, often blending modern biomedicine with traditional practices. In Kerala, India, for instance, patients incorporate Ayurvedic medicine and folk herbal remedies alongside conventional treatments, reflecting a holistic approach to health that honors cultural heritage. This amalgamation of healthcare practices highlights the necessity of acknowledging and integrating traditional health paradigms into modern healthcare solutions.
Furthermore, Goody [17]articulates the critical role that cultural food practices play in diabetes care and education. The application of frameworks such as the Campinha-Bacote Model of cultural competency is instrumental in enabling healthcare professionals to understand and respect the intricate relationship between cultural dietary habits and diabetes management. By recognizing and incorporating these cultural food practices into diabetes care, healthcare providers can develop more effective education and intervention strategies that align with patients’ lifestyles and beliefs.
These studies collectively underscore the potential for culturally tailored diabetes management applications to not only enhance their practical utility but also to resonate deeply with the daily lives and values of diverse patient populations. It is evident that there is a pressing need for such culturally informed tools, yet the current landscape reveals a scarcity of interventions that successfully integrate these critical cultural and traditional elements.
Considering this, our research is poised to fill a significant void by designing a healthcare intervention that not only acknowledges but prioritizes the cultural and traditional aspects of the Native American community. Our aim is to develop a diabetes management app that is not just functionally robust but also culturally attuned, ensuring that the Native American traditions and perspectives are interwoven into every facet of the app’s design and functionality.
3. Design
The development of a culturally sensitive diabetes self-management application for Native Americans necessitates a methodological approach that is both systematic and adaptive to the unique needs of the community. This study employed a community-based participatory research (CBPR) framework, which emphasizes collaboration and partnership with the target community at all stages of the app’s development. This approach aligns with the principles of respect, relevance, and reciprocity, ensuring that the research is culturally grounded and community driven.
Our methodology integrates qualitative data collection methods to inform the design and functionality of the mobile application. The process was iterative and responsive, allowing for continuous feedback and refinement. This section details the comprehensive steps taken—from participant recruitment, design considerations to app development. Each phase was conducted with rigorous attention to maintaining cultural integrity and fostering a sense of ownership and validation within the Native American community.
The core objective of our methodological design was to create an application that is not only a technological tool for diabetes management but also a culturally resonant resource that empowers Native American users and acknowledges their unique perspectives on health and well-being.
Our engagement with the Lower Sioux Indian Community indicated a sufficient level of access to smartphones and internet services, making the deployment of a mobile health app a viable option. This was corroborated by community feedback during the initial phase of our study, where participants expressed familiarity with and access to modern mobile technology. Thus, while acknowledging the existing challenges, our study operates on the premise that a significant portion of the target population has the means to access and benefit from the app, making it a relevant tool for diabetes self-care in these communities.
3.1. Background on Native American Traditions and Perspectives
In developing our study and the subsequent mobile application for diabetes self-care, we delved deeply into the rich tapestry of Native American traditions and perspectives. The Native American communities, with their diverse and vibrant cultural practices, offer a unique lens through which healthcare solutions can be viewed and tailored.
At the heart of our narrative is an understanding that health and wellness in Native American communities are not merely physical states but are deeply intertwined with spiritual, community, and environmental well-being. These aspects, often overlooked in conventional healthcare approaches, are central to the Native American perspective on health. Food is much more than sustenance in Native American cultures; it carries historical significance and is a medium for community bonding and cultural expression. Traditional foods, preparation methods, and communal eating practices are not only nutritional choices but also a means to preserve heritage and identity. We integrated these aspects to ensure our app respects and supports these dietary traditions. The role of family and community is paramount in Native American societies. Healthcare interventions, to be effective, must recognize and leverage these social structures. Our design process involved consultations with community members to understand how family dynamics and community interactions influence health behaviors and diabetes management. Storytelling, a revered tradition in Native American cultures, serves as an educational and cultural preservation tool. By incorporating elements of storytelling and native symbolism into our app, we aimed to connect users with their heritage, making the app not just a health tool but also a medium of cultural engagement.
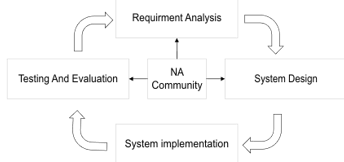
Figure 1: CBPR Process for Developing a Culturally Tailored Diabetes Management App
This narrative underscores our commitment to developing a diabetes self-management tool that is not only functionally effective but also culturally congruent. By incorporating these cultural insights, we aim to bridge the gap between technology and tradition, offering a healthcare solution that resonates deeply with Native American communities.
3.2. NA Community Based Participatory Research
Our research is deeply rooted in the principles of Community-Based Participatory Research (CBPR), an approach that ensures the development of our mobile application is closely aligned with
the distinct needs and cultural context of the Native American (NA) community. Figure 1 illustrates the cyclical and collaborative nature of the CBPR process, which integrates the Lower Sioux Indian Community throughout the system development cycle.
This study has been granted ethical approval by Lower Sioux Indian Community Tribe’s governance body under resolution number 16-153.
3.2.1. Requirement Analysis
In the initial phase of our study, a detailed requirement analysis was conducted, as illustrated by the top box of Figure 1. This phase was twofold: it involved individual interviews with domain experts and focused group sessions with the community.
We engaged in knowledge elicitation sessions with an assembly of domain experts, including tribal leaders from the Native American reservation community in the upper Midwest, local diabetes physicians, nutritionists specializing in diabetes care, and public health faculty. Preliminary meetings were convened to gather coarse-grained, general knowledge and set the foundation for a more nuanced understanding of the domain. The insights from these meetings were meticulously documented, serving as a vital reference for developing a domain-relevant ontology and for informing subsequent, more detailed inquiries.
Parallel to expert interviews, focused group discussions were held with members of the Lower Sioux Indian Community to explore the lived experiences of managing diabetes within their socio-cultural context. These sessions were pivotal in extracting nuanced insights into the community’s cultural traditions, resource accessibility, socio-economic factors, and the specific challenges encountered in diabetes self-management. The iterative nature of these discussions is signified by the two-way arrows in Figure 1, reflecting the dynamic exchange between the research team and the community, ensuring that their voices directly influenced the requirement analysis.
The amalgamation of knowledge from domain experts and the experiential wisdom of the community formed a comprehensive foundation for our requirement analysis. This collaborative approach ensured that the resulting diabetes self-management app was not only grounded in expert knowledge but also deeply embedded in the cultural and practical realities of the Native American users it seeks to serve.
3.2.2. Cultural Diversity in App Design
Our mobile app embraces the cultural diversity of Native American tribes and communities through an adaptable and inclusive design. The following features have been integrated:
- Dynamic Ontology-Based Foundation: Built on an extensible ontology, the app’s knowledge base is tailored to the Lower Sioux tribe but is designed to expand to include the cultural nuances of other tribes.
- Modular Design: This allows for the agile integration of tribe-specific content, ensuring that the app remains relevant across a spectrum of Native American cultures.
- Community Involvement: We leverage a community forum chatgroup function for direct input from users, ensuring the app’s cultural accuracy and responsiveness.
- Cultural Education and Sharing: The app promotes inter-tribal cultural exchange, enhancing understanding and unity among its users.
By incorporating these elements, our app is designed to be a culturally intelligent tool for diabetes self-management, adaptable to the varied practices and traditions of Native American communities.
3.2.3. System Design
With the input garnered from the community, we progressed to the System Design phase, which is shown on the right side of Figure 1. In this stage, we employed a participatory design methodology to mold the system’s interface, functionality, and features. Our design choices were culturally informed, integrating tribal logos and NA celebrity voices to ensure the application resonates with the community’s cultural heritage and preferences. The participatory nature of this phase is illustrated by the continuous loop back to the central community collaboration element in the figure, signifying an ongoing exchange of ideas and feedback.
3.2.3.1. Accessibility and Communication Strategy
Our mobile application has been meticulously crafted to facilitate effective communication and comprehension of health management strategies within the Native American community. During the design phase, input from tribal community members was sought to identify straightforward and easily understood terms, thereby avoiding intricate medical terminology.
Recognizing the potential obstacle that language can present, we have strategically reduced dependence on text. The application makes extensive use of intuitive visuals, symbols, and icons that are widely recognizable and can bridge linguistic gaps. These graphical elements are instrumental in effectively imparting health-related information.
In addition to visual aids, the application features an integrated natural voice assistant. This tool extends beyond mere navigation aid; it serves as an interactive medium for users who might favor auditory learning or those who find it more accessible. The voice assistant is programmed to communicate in a clear and comprehensible manner, catering to users with diverse literacy levels and language abilities.
In essence, our application overcomes language challenges by combining straightforward language, illustrative aids, and a user-friendly voice assistant, ensuring that all users, irrespective of their language proficiency, can easily access and understand health management strategies.
3.2.3.2. Socioeconomic Factors in App Design
Our mobile app is strategically designed to mitigate the socioeconomic challenges faced by Native American populations in managing diabetes. It provides personalized nutrition plans that are sensitive to users’ financial situations and the local availability of food, ensuring that the dietary recommendations are both affordable and accessible. The app respects and supports the inclusion of traditional Native American foods, fostering sustainable eating practices deeply rooted in cultural heritage. Recognizing the variety in health literacy levels, the app conveys information using straightforward language and visual aids to ensure comprehensibility for all users. A curated database within the app guides users to local, cost-effective options for diabetes-friendly meals and healthcare services. Additionally, community forums and groups within the app serve as platforms for sharing resources and strategies, reinforcing a network of support attuned to the users’ socioeconomic realities. This holistic approach to app design underscores our commitment to providing a supportive and accessible diabetes self-management tool for Native American communities.
3.2.3.3. Cultural User Centered Interface Design
Our approach adopts a Cultural-User-Centered Design (CUCD) approach to construct an interface meticulously crafted to resonate with Native American (NA) users. This design methodology is deeply rooted in cultural sensitivity, ensuring that the interface serves not just as a tool, but also as a cultural bridge. We’ve integrated a spectrum of culturally significant elements, each chosen for its profound connection to the NA community
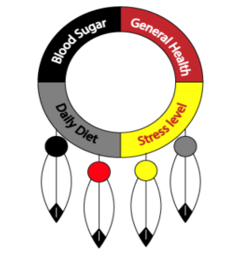
Figure 2: Tribal Emblem as UI Component

Figure 3: (a) Manual carb input Interface. (b) Calculated carb input through meal selection Interface (c) Voice assistant based Carb input
· Tribal Emblem Integration
The integration of the tribal emblem within our user interface serves as a cornerstone of our culturally tailored design strategy. This emblem shown in figure 2, segmented into four interactive quadrants, does more than provide aesthetic value; it functions as a dynamic interface element. Each quadrant is meticulously crafted to represent an essential component of the system’s functionality and to serve as a navigational aid, transforming into buttons that, upon interaction, reveal detailed logs and further information pertaining to the system’s various modules. The emblem itself is deliberately chosen for its cultural significance, embodying the rich heritage and shared history of the community. It acts as a visual anchor, grounding the user experience in familiar iconography that resonates on a personal level with the community members. Its inclusion is a thoughtful acknowledgment of the community’s values, traditions, and identity, intended to engender a sense of belonging and ownership over the technological experience.
This emblematic interface promotes accessibility and ease of use, with each interactive portion designed to guide users through the system’s capabilities intuitively. For instance, selecting one quadrant might reveal insights into the daily diet analysis data, while another might delve into blood sugar logs and trends over
time. This method of organization not only simplifies navigation but also aligns with the community’s cognitive patterns and cultural context, making the system’s operation inherently intuitive for the intended NA users. It’s a harmonious blend of function and tradition, ensuring that the system is not only efficient but also culturally congruent, facilitating a seamless and resonant user experience.
· Celebrity Vocal Engagements
To enrich the interface’s auditory experience, we have procured voice recordings from Native American luminaries and venerated figures, like Evan Adams, known for his pivotal portrayal of Thomas Builds-the-Fire in the seminal film “Smoke Signals.” His voice serves as a thread weaving through our interface, providing guidance and feedback, imbuing the user experience with authenticity and a deeper cultural linkage. This initiative goes beyond mere functionality—it is a homage to a voice that echoes the collective memories and experiences of the NA community.
· Linguistic Tailoring
Acknowledging the diverse linguistic capabilities within the NA communities, our interface offers customizable language options. It allows users to select their preferred language and adjust the complexity of the language to match their literacy level, ensuring accessibility and comprehension for all. Insights into this aspect of our design process are detailed in publication [18].
· Multi Modal Interaction
Our application offers a multifaceted interface designed to accommodate the distinctive communication styles within the community. As depicted in Figure 3(a), the app includes a straightforward graphical user interface for manual carbohydrate entry. This tactile method is uncomplicated, facilitating quick and direct input of carbohydrate consumption through simple screen interactions.
In another approach, demonstrated in Figure 3(b), the app leverages a sophisticated algorithm to estimate carbohydrate intake from meal selections. Users can describe their meals, and the app intelligently calculates and logs the carbohydrate content, streamlining the tracking process.
Additionally, Figure 3(c) introduces the convenience of a voice assistant. This modality allows users to verbally log their carbohydrate intake, accommodating those who might find manual entry cumbersome or prefer the immediacy of speech.
These three modalities reflect our dedication to inclusive design, offering both visual and auditory options to manage health data in the most intuitive way possible. By embracing diverse methods of interaction, the app not only improves user experience but also respects the cultural and individual preferences of our wide-ranging user demographic. This inclusive approach positions our application as a comprehensive tool for managing diabetes through user-friendly carbohydrate tracking.
· Cultural Narratives and Context
The interface weaves in narratives, traditions, and practices that are the fabric of NA cultural identity. These elements are not mere adornments; they serve to create a digital experience that is culturally congruent, fostering a sense of community and relevance.
The CUCD methodology champions the idea that an interface should be a cultural artifact, one that NA users can see themselves reflected in. By weaving these culturally rich threads into the interface, we aim to deliver an experience that is not only functionally superior but also culturally enriching and empowering for NA users.
3.2.3.1. Cultural Tailored System Design
In the development of our system, we prioritize a nuanced approach tailored to Native American (NA) users, focusing on elements that cater to their unique dietary needs and cultural practices. This includes:
Our system is finely tuned to offer personalized nutrition advice, considering the distinct dietary preferences and needs of NA users. We understand the importance of incorporating traditional and culturally significant foods in our recommendations. This includes a special emphasis on game food, which is not only a dietary staple but also holds deep cultural significance in many NA communities.
Recognizing the diverse culinary landscape across NA communities, our app considers the availability of local foods. This involves integrating traditional ingredients and dishes that are integral to various NA cultures, ensuring that our nutritional guidance is not only health-focused but also culturally resonant.
The socioeconomic context of NA communities is a critical aspect of our system design. We strive to make our nutritional recommendations affordable, considering the varying economic backgrounds of our users. This ensures that our guidance is realistic and accessible, not just theoretically ideal.
Our app goes beyond basic nutritional advice by embracing the rich cultural heritage of NA communities. We respect and incorporate traditional food practices and preferences, ensuring that our recommendations do not conflict with cultural norms and practices. Our app also acknowledges the diverse cultural practices and beliefs of tribal members, offering personalized lifestyle recommendations. For instance, we suggest physical activities like traditional dancing or nature walks on ancestral trails, which are not only enjoyable but also culturally significant. These suggestions honor the traditions and enhance the physical well-being of NA users.
To bridge the gap between nutritional advice and practical meal options, we analyze local restaurant menus. This analysis is geared towards ensuring that the food options available to NA users at local eateries are in line with their dietary requirements and cultural preferences. Previously our work [19–21]on restaurant menu and personized meal planning describes how health conditions can be used to recommend foods. This feature not only supports healthy eating habits but also promotes cultural integrity and relevance.
Understanding the centrality of family and community in NA culture, our app encourages social activities that strengthen these bonds. This could include family-based support systems or participation in cultural events and gatherings. By doing so, we aim to foster a supportive environment that is conducive to positive health outcomes and sustained user engagement.
Our social network feature is designed with a deep understanding of the importance of community connections in NA culture. It enables users to connect, share experiences, and support each other in their journey of diabetes self-management. This virtual community space is a platform for exchanging ideas, sharing cultural practices pertinent to diabetes management, and providing emotional support. It’s more than a network; it’s a communal space that strengthens the sense of belonging and encourages positive health behaviors.
We facilitate easy and meaningful communication between NA users and healthcare professionals who are attuned to their cultural context. This feature ensures that healthcare delivery is culturally competent, addressing the unique needs and preferences of NA users. It’s a bridge connecting users with healthcare providers in a way that respects and understands their cultural background.
The app provides educational content specifically tailored to the cultural sensitivities and needs of NA users. Covering various aspects of diabetes management, including diet, physical activity, medication, and self-monitoring, this content is not just informative but also relatable. It’s designed to be a culturally relevant guide in managing diabetes effectively.
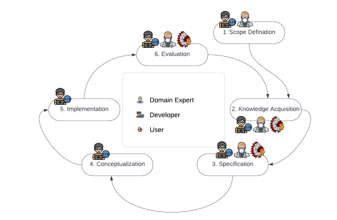
Figure 4: Ontology design and development life cycle
By incorporating features that facilitate effective communication and tailored education, our app plays a pivotal role in promoting culturally competent healthcare. It respects and acknowledges the influence of cultural context on health beliefs and behaviors, aiming to bridge any gaps between healthcare providers and users.
Overall, our system is meticulously designed to provide a relevant, inclusive, and culturally sensitive user experience for NA users. It aims to promote healthy lifestyle changes, foster community support, and ultimately contribute to improved health outcomes within the NA community. Our approach is not just about managing diabetes; it’s about embracing and integrating the rich cultural heritage of NA users into every aspect of their healthcare journey.
3.3. NA Biocultural Profile Ontology Development
In designing self-management solutions for diabetes within Native American (NA) populations, it is essential to acknowledge and integrate their distinct biocultural attributes. Our approach introduces a sophisticated biocultural user profile ontology, NAOnto, tailored to encapsulate the intricate tapestry of biological, cultural, socio-economic, and environmental factors that characterize NA diabetes patients. This ontology is a rich repository of data points, including but not limited to cultural influences, geographic locations, prevalent health beliefs and attitudes, varying literacy and numeracy levels, physical capabilities, familial support structures, and economic conditions. Together, these variables form a holistic view of a patient’s well-being, firmly rooted in their unique biocultural landscape.
The creation of NAOnto was orchestrated through a structured six-phase process, as depicted in Figure 4. Beginning with scope definition, our team delineated the boundaries and objectives of the ontology, ensuring alignment with the specific self-management needs of NA diabetes patients. Subsequent knowledge acquisition involved meticulous gathering of information from a host of resources, including direct inputs from the community and domain experts. Specification followed, where the acquired knowledge was translated into a detailed framework, leading to the conceptualization phase, which established the ontology’s foundational structures and relationships.
In the course of development, we have collaborated with the Community Health & Social Service Directors, the Clinic CEO, and two of their assistants from the Lower Sioux Indian Community. While these professionals did not participate in the broader user validation process, they played a crucial role during the design phase. Their insights and contributions were pivotal in tailoring our app’s design to be culturally sensitive and to address the specific healthcare needs of the Native American community.
To ensure a wider relevance and applicability, a survey-based user study with nine participants was conducted across Native American communities in North Dakota and Minnesota.
The implementation phase saw the ontology being constructed and populated with data, while the evaluation phase subjected it to rigorous community and expert review, allowing for validation and calibration against real-world scenarios. This cyclical development process—iterative in nature—permitted ongoing refinement and updating of the ontology, ensuring that it remained dynamic and reflective of the evolving understanding of the NA community’s needs and the latest medical insights. The result is a dynamic, living model that is as responsive as it is comprehensive.
The utility of NAOnto extends beyond a mere database; it is a critical tool for crafting personalized diabetes self-management strategies that honor the biocultural context of NA patients. Through NAOnto, we enable the creation of interventions that are not only medically precise but also culturally consonant, fostering greater acceptance and effectiveness.
Figure 5 presents a partial view of the NAOnto that is defined for this research. Further details of the ontology’s structure and its application within our CBPR framework are elaborated in the accompanying publications [22,23], where we delve into the granularities of NAOnto and its operational impact.
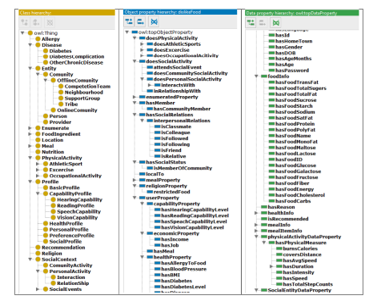
Figure 5: Partial view of ontology NAOnto
4. Implementation
The development and deployment of our diabetes self-management mobile app leveraged the capabilities of the Ionic framework and Javalin server, optimizing it for both functionality and security.
Ionic was selected for its exceptional cross-platform capabilities, allowing us to create a single codebase that functions seamlessly on both iOS and Android platforms. This choice significantly streamlined the development process, ensuring a consistent user experience across different devices.
Javalin, a lightweight Java and Kotlin web framework, was employed for handling HTTP requests between the app and our backend server. It efficiently routes these requests to the appropriate handlers, ensuring swift and accurate data processing.
To safeguard user data, all communications between the mobile app and the Javalin server were encrypted using HTTPS protocols. Additionally, data stored on the SQL server was secured using RSA encryption, reflecting our commitment to data security and user privacy.
The app features several unique interfaces, each designed with specific user needs in mind. In figure 6(a) shows the integration of the Lower Sioux tribal logo into our diabetes management system offers a culturally sensitive and intuitive interface. The health
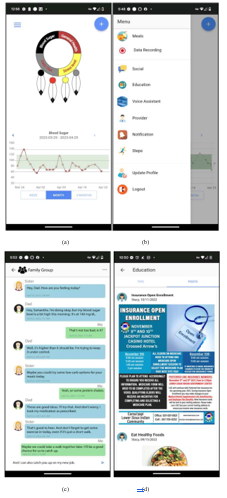
Figure 6: Screenshots of the mobile app.
wheel, divided into sections representing blood sugar levels, general health, stress levels, and diet, allows users to input and track their data efficiently. In figure 6(b) menu encompasses a broad range of features including meal recommendations, health data recording, social networking, educational resources, and direct connectivity with healthcare providers. It’s a holistic state of tools designed to facilitate diabetes self-management. Family Group Communication Feature is shown in figure 6(c) Acknowledging the importance of family in NA culture, this feature enables family members to support each other in diabetes management, promoting a collaborative care approach. Culturally feature enables family members to support each other in diabetes management, promoting a collaborative care approach. Culturally Tailored Education and Events is shown in figure 6(d). This aspect of the app keeps users informed about cultural events and educational resources, fostering community engagement and participation.
Each app function underwent rigorous testing to ensure optimal performance and usability. We conducted multiple use case studies to assess the feasibility and effectiveness of features such as meal planning and restaurant menu recommendations. Specific app functions like personalized meal planning and restaurant menu screening were evaluated through user studies. These studies provided insights into the usability and impact of these features on the self-management of diabetes among NA users.
While individual functions have been evaluated, a comprehensive assessment by the tribal community is pending. We plan to engage with the Lower Sioux community to gather feedback and assess the overall effectiveness of the app. This evaluation will offer vital insights into the app’s acceptability, practicality, and its impact on health outcomes in the NA community.
To ensure sustained engagement with our mobile app, we have developed a comprehensive strategy focusing on personalization, gamification, community involvement, and continuous improvement. Personalization is key; the app learns and adapts to user interactions, offering tailored recommendations to maintain relevance. Gamification techniques, such as challenges and rewards, are introduced to engage users and encourage consistent app usage. As part of our cyclical Community-Based Participatory Research (CBPR) process, depicted in Figure 1, we commit to regular content updates, providing fresh information and resources that invite users to keep engaging with the app. Community features like forums and support groups are incorporated to cultivate a supportive network, enhancing user motivation through shared experiences and successes. Additionally, we have established a feedback mechanism that enables users to contribute to the app’s evolution, ensuring it continuously aligns with their preferences and needs. This strategic approach aims to integrate the app into users’ daily routines, making it a valuable, long-term asset in diabetes self-management.
In summary, our diabetes self-management app combines technological innovation with cultural sensitivity. It’s designed not just as a tool for health management, but as a culturally attuned companion for Native Americans. Our goal is to empower users through a blend of modern technology and respect for traditional values and practices, thereby facilitating effective diabetes management in the NA community.
5. Conclusion
In the concluding section of our paper, we emphasize the successful design and development of a mobile application that is specifically tailored to the needs and cultural nuances of Native Americans (NAs) with diabetes. Our approach, characterized by a deeply collaborative and iterative design process, incorporated valuable insights from the Lower Sioux Indian Community. This collaboration was instrumental in shaping an app that is not only technologically sound but also deeply respectful and reflective of the unique cultural traditions, local resources, and socio-economic realities of the NA population.
The app offers bespoke dietary recommendations, aligning with the traditional dietary habits and available local food resources of NAs. This personalized approach ensures that the guidance is not only health-conscious but also culturally appropriate. Acknowledging the integral role of family in NA communities, the app incorporates features that enable and encourage family involvement in diabetes management, promoting a collective approach to health and wellness. The app provides users with information on local resources, including traditional foods and community events, facilitating a connection between users and their local environment. By embedding cultural elements into the app’s interface and functionality, we ensure that the technology resonates with the users on a cultural level, enhancing engagement and relevance.
Moving forward we aim to conduct extensive user studies within the Lower Sioux community. These studies will involve a larger sample size to ensure a more diverse and representative feedback. A key focus of our upcoming studies will be to evaluate the app’s effectiveness in improving health outcomes among NAs with diabetes. This will involve tracking various health indicators and user engagement metrics over time. The feedback obtained from these comprehensive studies will be pivotal in further refining the app. Our goal is to continuously evolve the app’s features and usability to better align with the needs and preferences of NA users. While our initial focus has been on the Lower Sioux community, we envisage expanding the reach of the app to other NA communities, adapting it to different tribal traditions and needs.
In summary, our paper not only details the creation of a culturally tailored mobile app for NAs with diabetes but also sets a roadmap for its future development and enhancement. By continuing to engage with the community and rigorously assessing the app’s impact, we aim to create a dynamic tool that not only supports diabetes management but also fosters a deeper connection between health technology and cultural identity. This endeavor reflects our commitment to developing solutions that are not only technologically advanced but also culturally empathetic and responsive to the unique needs of diverse populations.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
The authors express their gratitude to Dr. Donald Warne, Darin Prescott, Stacy Hammer and the Lower Sioux Indian community for their invaluable support, collaboration, valuable suggestions, and feedback. Their contribution has been instrumental in the development and improvement of our app, and we are thankful for their ongoing partnership and commitment to improving healthcare outcomes for Native American communities affected by diabetes. This work was supported by the National Science Foundation (NSF) with award numbers: 1722913 and 2218046.
- National Diabetes Statistics Report | Diabetes | CDC, Jan. 2024.
- Disparities | Fact Sheets, Jan. 2024.
- A.H. Ariel-Donges, E.L. Gordon, B.N. Dixon, A.J. Eastman, V. Bauman, K.M. Ross, M.G. Perri, “Rural/urban disparities in access to the National Diabetes Prevention Program,” Translational Behavioral Medicine, 10(6), 1554–1558, 2020, doi:10.1093/TBM/IBZ098.
- M. Sarche, P. Spicer, “Poverty and health disparities for American Indian and Alaska native children: Current knowledge and future prospects,” Annals of the New York Academy of Sciences, 1136, 126–136, 2008, doi:10.1196/ANNALS.1425.017.
- R. Struthers, F.S. Hodge, B. Geishirt-Cantrell, L. De Cora, “Participant Experiences of Talking Circles on Type 2 Diabetes in Two Northern Plains American Indian Tribes,” Http://Dx.Doi.Org/10.1177/1049732303256357, 13(8), 1094–1115, 2003, doi:10.1177/1049732303256357.
- C.O. Airhihenbuwa, C.L. Ford, J.I. Iwelunmor, “Why Culture Matters in Health Interventions,” Http://Dx.Doi.Org/10.1177/1090198113487199, 41(1), 78–84, 2013, doi:10.1177/1090198113487199.
- M.W. Kreuter, S.N. Lukwago, D.C. Bucholtz, E.M. Clark, V. Sanders-Thompson, “Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches,” Http://Dx.Doi.Org/10.1177/1090198102251021, 30(2), 133–146, 2003, doi:10.1177/1090198102251021.
- M. Barrera, F.G. Castro, L.A. Strycker, D.J. Toobert, “Cultural adaptations of behavioral health interventions: a progress report,” Journal of Consulting and Clinical Psychology, 81(2), 196–205, 2013, doi:10.1037/A0027085.
- A.L. Asad, T. Kay, “Toward a multidimensional understanding of culture for health interventions,” Social Science & Medicine, 144, 79–87, 2015, doi:10.1016/J.SOCSCIMED.2015.09.013.
- A. Quevedo Rodríguez, A.M. Wägner, “Mobile phone applications for diabetes management: A systematic review,” Endocrinología, Diabetes y Nutrición, 66(5), 330–337, 2019, doi:10.1016/J.ENDINU.2018.11.005.
- P.P. Brzan, E. Rotman, M. Pajnkihar, P. Klanjsek, “Mobile Applications for Control and Self Management of Diabetes: A Systematic Review,” Journal of Medical Systems, 40(9), 1–10, 2016, doi:10.1007/S10916-016-0564-8/METRICS.
- S. Sneha, S. Thalla, I. Rischie, H. Shahriar, “Health Internet Technology for Chronic Conditions: Review of Diabetes Management Apps,” Jan. 2024, doi:10.2196/17431.
- M.M. Kebede, C.R. Pischke, “Popular diabetes apps and the impact of diabetes app use on self-care behaviour: A survey among the digital community of persons with diabetes on social media,” Frontiers in Endocrinology, 10(MAR), 135, 2019, doi:10.3389/FENDO.2019.00135/BIBTEX.
- F. Petersen, “Impact of Culture on the Adoption of Diabetes Self-Management Applications: Cape Flats, South Africa,” ArXiv.Org, 2021.
- A. Millan-Ferro, A.E. Caballero, “Cultural approaches to diabetes self-management programs for the Latino community,” Current Diabetes Reports, 7(5), 391–397, 2007, doi:10.1007/S11892-007-0064-9/METRICS.
- E. Chacko, “Culture and therapy: complementary strategies for the treatment of type-2 diabetes in an urban setting in Kerala, India,” Social Science & Medicine, 56(5), 1087–1098, 2003, doi:10.1016/S0277-9536(02)00105-3.
- C.M. Goody, L. Drago, “Using Cultural Competence Constructs to Understand Food Practices and Provide Diabetes Care and Education,” Diabetes Spectrum, 22(1), 43–47, 2009, doi:10.2337/DIASPECT.22.1.43.
- R. Hendawi, S. Alian, J. Li, “A Smart Mobile App to Simplify Medical Documents and Improve Health Literacy: System Design and Feasibility Validation,” Jan. 2024, doi:10.2196/35069.
- B. Maharjan, J. Li, J. Kong, C. Tao, “Alexa, What Should I Eat? : A Personalized Virtual Nutrition Coach for Native American Diabetes Patients Using Amazon’s Smart Speaker Technology,” 2019 IEEE International Conference on E-Health Networking, Application and Services, HealthCom 2019, 2019, doi:10.1109/HEALTHCOM46333.2019.9009613.
- M.S.A.T. Zadeh, J. Li, S. Alian, “Personalized Meal Planning for Diabetic Patients Using a Multi-Criteria Decision- Making Approach,” 2019 IEEE International Conference on E-Health Networking, Application and Services, HealthCom 2019, 2019, doi:10.1109/HEALTHCOM46333.2019.9009593.
- W. Ul Hasan, K. Tuz Zaman, M.S.A.T. Zadeh, J. Li, “Eat This, Not That! – a Personalised Restaurant Menu Decoder That Helps You Pick the Right Food,” 2022 IEEE International Conference on E-Health Networking, Application and Services, HealthCom 2022, 43–48, 2022, doi:10.1109/HEALTHCOM54947.2022.9982770.
- V. Pandey, J. Li, S. Alian, “Evaluation and Evolution of NAOnto – An Ontology for Personalized Diabetes Management for Native Americans,” 2021 7th International Conference on Computer and Communications, ICCC 2021, 1635–1641, 2021, doi:10.1109/ICCC54389.2021.9674339.
- J. Li, S. Alian, “Design and development of a biocultural ontology for personalized diabetes self-management of American Indians,” 2018 IEEE 20th International Conference on E-Health Networking, Applications and Services, Healthcom 2018, 2018, doi:10.1109/HEALTHCOM.2018.8531107.
No. of Downloads Per Month
No. of Downloads Per Country
