Verify of Left and Right Differences in Sleep Index using the Ring-type Sensor
Volume 9, Issue 1, Page No 9-14, 2024
Author’s Name: Yutaka Yoshida, Emi Yudaa)
View Affiliations
Tohoku University, Graduate School of Information Sciences, Sendai, 980-8579, Japan
a)whom correspondence should be addressed. E-mail: yuda@ieee.org
Adv. Sci. Technol. Eng. Syst. J. 9(1), 9-14 (2024); ![]() DOI: 10.25046/aj090102
DOI: 10.25046/aj090102
Keywords: Ring type wearable sensor, Sleep index, Left and right difference
Export Citations
In this study, two healthy women in their 40s wore Oura Rings on both fingers and verified left and right differences in sleep index. Bed time, sleep time, rem sleep, sleep score, and heart rate had small left and right differences in both subjects, and a high correlation of 0.8 or more was observed(subjectA:P<0.001,subjectB:P<0.01). Subject B showed a significant difference in the mean values of sleep latency, awakening time and sleep efficiency, and one finger was overestimated(P<0.05). Although the detection accuracy of sleep stages differs depending on the stage, it was shown that the influence of left and right differences is particularly small for bed time, sleep time, rem sleep, sleep score and heart rate.
Received: 20 October 2023, Revised: 19 December 2023, Accepted: 19 December 2023, Published Online: 20 January 2024
1. Introduction
This paper is an extension of the 2022 World Automation Congress presentation [1]. Recent ring-shaped sensors can non-invasively measure heart rate, body surface temperature, and body acceleration. Indexes related to sleep time and sleep quality can also be calculated and visualized using a smartphone application. Among ring-shaped sensors, the Oura Ring has received particular attention in recent years and has been verified the accuracy of detecting HRV (heart rate variability) index and sleep stages during sleep using a combination of Electrocardiogram (ECG) and polysomnography (PSG) [2-5]. In addition, studies have been reported on accuracy comparisons with other wearable devices [6-9] and long-term tracking of physiological characteristics related to menstrual cycles and sleep [10].
In a study on accuracy evaluation regarding the wearing position of wearable sensors, it has become clear that the index obtained from wristwatch-type sensors varies depending on the wearing position [11], making it somewhat difficult to evaluate a stable index. However, there are no study reports that examine the left and right differences in the index when the Oura Ring is worn on both fingers.
Therefore, in this study, we wore Oura Ring to both fingers to record biological signals during sleep and verified left and right differences in sleep index calculated by the application.
2. Method
2.1. Experimental protocol
Subjects were two healthy women (subjectA:42y.o., subjectB:41 y.o.). The gist of the study was explained to the two subjects, and consent was obtained. The studies involving human participants were reviewed and approved by Center for Data-driven Science and Artificial Intelligence Tohoku University Institutional Review Board (No.2022-6, Approved 25 August, 2022).
Before going to bed, the subjects wore two ring type wearable sensor on both index fingers to record their sleep index for the night. The measurement period was from January 25, 2022 to October 24, 2022, with 172 days of data for Subject A and 10 days for Subject B. The measurements were not performed consecutively every day, but the subjects were allowed to decide for themselves, and the experiment was performed without straining while taking into account the prevention of skin irritation.
2.2. Ring type wearable sensor
The ring-type wearable sensor used Oura Ring Generation 3(Oura, Inc., USA). Oura Ring has 15 sensors inside a titanium ring and can measure biological information such as heart rate, skin temperature, physical activity, and sleep index.

Figure 1: Oura Ring Generation 3
Pulse wave measurement uses an LED light sensor. Infrared and red LED run in dark places because they are more affected by ambient light, and green LED runs in bright places because they are less affected by ambient light. These sensors measure the amount of blood flow (change in blood vessel volume) that

Figure 2: State of charging
changes with the pulse of the heart. Relative temperature is measured with an NTC (negative temperature coefficient) thermistor. Physical activity and body motion are measured with the 3-axis accelerometer. The measured biological information is transferred to the Oura application via Bluetooth and output to a CSV file.
The size is 6 to 13 (ring width 7.8mm), and the weight is 4 to 6g. Battery life is 5-7 days, charging time is 20-80 minutes, and memory capacity is 16MB. The outside temperature range for use is -10℃ to 52℃.
2.3. Sleep index and Statistical analysis
The sleep index is shown in Table 1. Heart rate is the average heart rate for 5 minutes, and respiratory rate is measured only once during one sleep. Mean values, standard deviations, and correlation coefficients of sleep indices obtained from both fingers were calculated. Mean values were compared by Paired t-test. The significance level was set at 5%, and significant at P < 0.05.
3. Results
Table 1 shows the statistical results of the sleep index of the two subjects. For subject A, there was no significant difference between the left and right mean values, but significant correlations were observed in all indices (P<0.001). However, the strength of the correlation varies by index. In particular, bed time, sleep time, shallow non-rem, rem sleep, sleep score, heart rate and respiration rate showed a high correlation of 0.8 or more. On the other hand, subject B showed a significant difference in the mean values of sleep latency, awakening time and sleep efficiency, and one finger was overestimated (P<0.05). Bed time, sleep time, rem sleep, awakening time, sleep efficiency, sleep score and heart rate showed a significant correlation of 0.8 or more (P<0.01). Bed time, sleep time, rem sleep, sleep score, and heart rate were highly correlated with small left and right differences in both subjects.
Figure 3 and figure 4 are scatter plots of the left and right finger sleep indices for subject A and subject B, respectively. The vertical axis is the right finger and the horizontal axis is the left finger. In subject A, the distribution of sleep latency was such that the longer the right finger, the shorter the left finger, or the longer the left finger, the shorter the right finger. Awakening time and sleep efficiency had a square distribution. In subject B, the sleep latency was longer with the right finger than with the left. There is a high correlation of awakening time and sleep efficiency, but awakening time was longer with the right finger, and the sleep efficiency was greater with the left finger, resulting in a bias.
4. Discussion
There are many reports on the accuracy evaluation of HRV and sleep stages measured by Oura Ring during night sleep.
Reference [2] reported detection accuracy of 65%, 51%, and 61% for shallow sleep, deep sleep, and rem sleep, respectively. A study using machine learning combined accelerometers, body temperature, and HRV to detect four stages of light NREM sleep, deep NREM sleep, REM sleep, and wake with 79% accuracy[3].Studies comparing HRV parameters during nocturnal sleep using ECG and Oura Ring have shown very high heart rate correlations during the night, indicating that HR can be measured with high accuracy [4,5]. A study comparing TST (total sleep time) between Samsung Gear Sport watches and Oura Ring showed a correlation of 0.86, and the average difference was within an acceptable range [7]. Based on the results of these previous studies, the cause of the difference between the left and right is thought to be the movement of the fingers and the detection accuracy of the device’s algorithm. Since heart rate is detected as an average heart rate over a 5-minute period, there may be some fluctuations from beat to beat, but when looking at the baseline (average value) of heart rate, the difference between the left and right becomes smaller.
Table 1: Sleep index
| Bedtime (min) | Awakening time (min) |
| Sleep time (min) | Sleep efficiency (%) |
| Sleep latency (min) | Sleep score |
| Shallow non-rem (min) | Heart rate (bpm) |
| Deep non-rem (min) | Respiration rate (frequency/min) |
| Rem sleep (min) | Relative body temperature (℃) |
Table 2: Statistical results of the sleep index.
| Sleep index | Subject A | Subject B | ||||||
| R-L | Mean±S.D. | Correlaion | R-L | Mean±S.D. | Correlaion | |||
| r | P-value | r | P-value | |||||
| Bed time (min) | R | 403±89 | 0.843 | <0.001 | R | 461±107 | 0.832 | 0.003 |
| L | 404±82 | L | 437±97 | |||||
| Sleep time (min) | R | 339±68 | 0.917 | <0.001 | R | 375±68 | 0.815 | 0.004 |
| L | 339±67 | L | 373±68 | |||||
| Sleep latency (min) | R | 11±9 | 0.195 | <0.001 | R | 14±10* | 0.529 | <0.001 |
| L | 11±9 | L | 7±4 | |||||
| Shallow non-rem (min) | R | 194±48 | 0.812 | <0.001 | R | 218±63 | 0.577 | 0.081 |
| L | 197±45 | L | 211±47 | |||||
| Deep non-rem (min) | R | 40±21 | 0.590 | <0.001 | R | 33±17 | 0.324 | 0.362 |
| L | 38±20 | L | 42±21 | |||||
| Rem sleep (min) | R | 105±33 | 0.845 | <0.001 | R | 123±28 | 0.800 | 0.006 |
| L | 103±33 | L | 119±32 | |||||
| Awakening time (min) | R | 64±36 | 0.500 | <0.001 | R | 87±49* | 0.837 | 0.003 |
| L | 65±34 | L | 64±50 | |||||
| Sleep efficiency (%) | R | 85±6 | 0.368 | <0.001 | R | 82±6* | 0.824 | 0.003 |
| L | 84±7 | L | 87±8 | |||||
| Sleep score | R | 66±9 | 0.848 | <0.001 | R | 70±8 | 0.861 | <0.001 |
| L | 66±10 | L | 72±8 | |||||
| Heart rate (bpm) | R | 63.38±3.63 | 0.994 | <0.001 | R | 64.97±4.50 | 0.870 | 0.001 |
| L | 63.39±3.67 | L | 63.63±4.05 | |||||
| Respiration rate (frequency/min) | R | 15.87±0.45 | 0.828 | <0.001 | R | 15.31±0.78 | 0.224 | 0.534 |
| L | 15.85±0.43 | L | 15.66±0.40 | |||||
| Relative body temperature (℃) | R | -0.03±0.26 | 0.735 | <0.001 | R | 0.05±0.25 | 0.612 | 0.06 |
| L | -0.03±0.27 | L | -0.03±0.27 | |||||
*P<0.05(right finger vs. left finger)
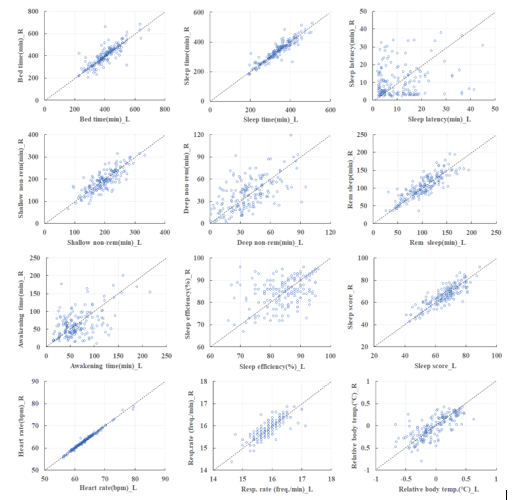
Figure 3: Scatter plots of the left and right finger sleep index for subject A.
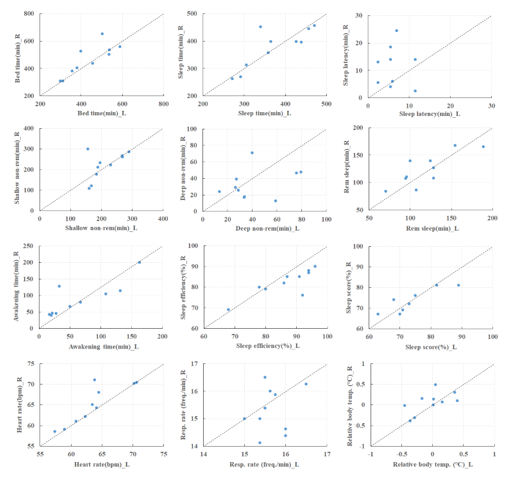
Figure 4: Scatter plots of the left and right finger sleep index for subject B.
In rem sleep, sympathetic nerve activity predominates, and the heart rate increases, whereas in non-rem sleep, parasympathetic nerve activity predominates and the heart rate decreases [12]. Therefore, the stages of rem sleep and non-rem sleep are easily detected, and the left and right differences in rem sleep are particularly small. The accuracy of detecting the shallow non-rem and deep non-rem stages is likely to decrease, and large differences between the left and right sides may occur. On the other hand, heart rate fluctuations are stable during non-rem sleep, but it is difficult to detect the difference between shallow non-rem and deep non-rem. The left and right difference in non-rem sleep may also be due to the algorithm.
Awakening time is the time for turning over in bed, arousal during sleep, and although the Oura Ring’s detection algorithm is unknown, it is thought that the acceleration sensor is involved in determining these times. Sleep efficiency is calculated as the ratio of total sleep time to bed time [13-15], and the longer the Awakening time, the more the sleep time is lost, and the lower the sleep efficiency. Therefore, bias occurs due to the difference in movement between the left and right fingers. In subject B, the right finger had a longer awakening time, so it is thought that sleep efficiency was lower on the right and higher on the left.
Heart rate measured by the Oura Ring during night sleep is measured with high accuracy, and furthermore, it is suggested that wearing it on the left and right fingers does not affect the measurement accuracy. Although the detection accuracy of sleep stages differs depending on the stage, it was shown that the influence of left and right differences is particularly small for bed time, sleep time, rem sleep, sleep score and heart rate.
5. Conclusion
The left and right differences in sleep index obtained from the Oura Ring were verified. There were small left and right differences in bed time, sleep time, rem sleep, sleep score, and heart rate. It is suggested that indices can objectively and accurately evaluate sleep quality and fatigue recovery for health promotion. Other indicators are thought to differ between left and right depending on the individual, and it is necessary to take these differences into account when evaluating sleep. In addition, the subjects’ health conditions, skin conditions such as wet skin or dry skin, and body positions during sleep were not recorded in this experiment, so indicators with large variations could not be categorized and analyzed. Considering these things, we will examine the effects of age and gender differences by increasing the number of subjects.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
This work was supported by a Grant-in-Aid for Strategic intellectual property/standardization, commercialization promotion support project for the Beyond 5G era from Ministry of Internal Affairs and Communications, Japan and the New Energy and Industrial Technology Development Organization (NEDO) Intensive Support for Young Promising Researchers Foundation.
- Y.Yoshida, H.Sakamoto, E.Yuda, “ Precision of human workout-time detection using Random Forests and Wearable Sensor Data,” 2022 World Automation Congress Proceedings, 429-432, 2022, doi:10.23919/WAC 55640.2022.9934354.
- M.D. Zambotti, L.Rosas, I.M.Colrain, F.C. Baker, “The Sleep of the Ring: Comparison of the ŌURA Sleep Tracker Against Polysomnography,” Behavioral Sleep Medicine, 17(2), 124-136, 2019, doi:10.1080/15402002.2017.1300587.
- M.Altini, H.Kinnunen, “The Promise of Sleep: A Multi-Sensor Approach for Accurate Sleep Stage Detection Using the Oura Ring,”Sensors (Basel), 21(13), 4302, 2021, doi: 10.3390/s21134302.
- R.Cao, I.Azimi, F.Sarhaddi, H.N.Vilen, A.Axelin, P.Liljeberg, A.M. Rahmani,“Accuracy Assessment of Oura Ring Nocturnal Heart Rate and Heart Rate Variability in Comparison With Electrocardiography in Time and Frequency Domains: Comprehensive Analysis,” Journal of Medical Internet Research, 24(1), e27487, 2022, doi:10.2196/27487.
- H.Kinnunen, A.Rantanen, T.Kenttä, H.Koskimäki,“Feasible assessment of recovery and cardiovascular health: accuracy of nocturnal HR and HRV assessed via ring PPG in comparison to medical grade ECG,Physiological Measurement”, 41(4), 04NT01, doi: 10.1088/1361-6579/ab840a.
- D.J.Miller, C.Sargent, G.D.Roach, “A Validation of Six Wearable Devices for Estimating Sleep, Heart Rate and Heart Rate Variability in Healthy Adults,” Sensors (Basel), 22(16), 6317, 2022, doi:10.3390/s22166317.
- M.A.Mehrabadi, I.Azimi, F.Sarhaddi, A.Axelin, H.N.Vilén, S.Myllyntausta, S.Stenholm , N.Dutt, P.Liljeberg , A.M.Rahmani, “Sleep Tracking of a Commercially Available Smart Ring and Smartwatch Against Medical-Grade Actigraphy in Everyday Settings: Instrument Validation Study, ” JMIR Mhealth Uhealth, 8(10), e20465, 2020, doi:10.2196/20465.
- E.D.Chinoy, J.A.Cuellar, J.T.Jameson, R.R.Markwald,“Performance of Four Commercial Wearable Sleep-Tracking Devices Tested Under Unrestricted Conditions at Home in Healthy Young Adults,” Nature and Science of Sleep, 14, 493-516, 2022, doi:10.2147/NSS.S348795.
- L.Nauha, V.Farrahi, H.Jurvelin, T.Jämsä, M.Niemelä, M.Kangas, R.Korpelainen, “Comparison and agreement between device-estimated and self-reported sleep periods in adults,” Annals of Medicine,55(1),2191001,2023,doi:10.1080/07853890.2023.2191001.
- E.Alzueta, M.D.Zambotti, H.Javitz, T.Dulai, B.Albinni, K.C.Simon, N.Sattari, J.Zhang, A.Shuster, S.C.Mednick, F.C.Baker,“Tracking Sleep, Temperature, Heart Rate, and Daily Symptoms Across the Menstrual Cycle with the Oura Ring in Healthy Women,” International Journal of Women’s Health, 14, 491-503,2022, doi:10.2147/IJWH.S341917.
- E.Yuda, K.Yamamoto, Y.Yoshida, J.Hayano, “Differences in pulse rate variability with measurement site,” Journal of Physiological Anthropology, 39(1), 4, 2020, doi:10.1186/s40101-020-0214-1.
- M.Yoshimoto, I.Yoshida, K.Miki,“Functional role of diverse changes in sympathetic nerve activity in regulating arterial pressure during REM sleep,” Sleep, 34(8),1093-1101,2011,doi:10.5665/SLEEP.1168.
- B.V.Vaughn, S.R.Quint, J.A.Messenheimer, K.R.Robertson,“Heart period variability in sleep,”Electroencephalogr Clin Neurophysiol, 94(3), 155-162,1995, doi:10.1016/0013-4694(94)00270-u
- P.Busek, J.Vanková, J.Opavský, J.Salinger, S.Nevsímalová,“Spectral analysis of the heart rate variability in sleep,” Physiological Research, 54(4), 369-376,2005.
- D.L.Reed, W.P.Sacco,”Measuring Sleep Efficiency: What Should the Denominator Be? ,” Journal of Clinical Sleep Medicine, 12(2), 263–266, 2016, doi:10.5664/jcsm.5498.
