Smart Healthcare Kit for Domestic Purposes
Volume 8, Issue 3, Page No 170-177, 2023
Author’s Name: Yehan Kodithuwakku1, Chanuka Bandara1, Ashan Sandanayake1, R.A.R Wijesinghe2, Velmanickam Logeeshan3,a)
View Affiliations
1Department of Electrical, Electronic and Telecommunication Engineering, Faculty of Engineering, General Sir John Kotelawala Defence University, Sri Lanka
2Department of Mechanical Engineering, Faculty of Engineering, General Sir John Kotelawala Defence University, Sri Lanka
3Department of Electrical Engineering, Faculty of Engineering, University of Moratuwa, Sri Lanka
a)whom correspondence should be addressed. E-mail: logeeshanv@uom.lk
Adv. Sci. Technol. Eng. Syst. J. 8(3), 170-177 (2023); ![]() DOI: 10.25046/aj080319
DOI: 10.25046/aj080319
Keywords: COVID-19, Beats per Minute, SpO2, Electrocardiogram, Telemedicine, Telehealth, Vital signs, Healthcare Kit
Export Citations
The COVID-19 pandemic has caused a substantial death toll throughout the world. The pandemic has created a threat to public health, the economy, food systems, and the workplace. An increased reprioritization of health expenditure towards COVID-19 vaccines will impact on allocations to other medical facilities. In developing countries, hospitals shortage the infrastructure to facilitate patients. Therefore, traditional checkups and clinics are not practical. According to research done in this article, 95 percent would prefer telemedicine and telehealth rather than conventional inspections. Even though smart healthcare technology has been implemented, it does not show adequate effectiveness when commercialized. Therefore, in this paper, a microcontroller-based, low-cost, automated, real-time system has been proposed to give a convenient solution for measuring the vital signs of the body. In this project, Multiple sensors with a microcontroller were intended to measure heartbeats per minute, Oxygen Saturation, body temperature and electrocardiogram of a patient at home without going to a hospital. The developed system indicated very less percentage error in temperature measurement and was able to maintain high accuracy on Beats per Minute, Oxygen Saturation and Electrocardiogram. This approach provides a feasible solution for both patients and medical professionals.
Received: 01 January 2023, Accepted: 20 March 2023, Published Online: 12 June 2023
1. Introduction
The goal of this article is to propose a revised and expanded version of the IoT-based Healthcare Kit for Domestic Use, which was first presented at the World AI(Artificial Intelligence) IoT(Internet of Things) Congress in 2022 [1]. Additional research and testing have been carried out in order to improve the device and provide more detailed explanations of its performance and efficiency. This document summarizes the most recent findings and conclusions from the smart healthcare kit’s ongoing research, development, and testing.
Since the start of the Coronavirus Disease 2019 (COVID-19) outbreak in early Wuhan in December 2019, it has spread to every country, including those with a low income [2]. It is possible that all nations will be vulnerable to this catastrophe as the world becomes a smaller, more integrated “global village.” As a result, the entire world is at risk if a pandemic cannot be stopped in one nation. Not only has a pandemic had a harmful impact on the health sector, but it has also caused difficult economic, social, and political crises that, if they are not resolved quickly, will leave lasting scars [3].
Recent analysis shows that patients with COVID-19 frequently have an increase in severity or death due to related illnesses like hypertension, diabetes, obesity, cardiac diseases etc[2]. The prevalence of chronic diseases is higher in low and middle-income countries due to several risk factors, including dietary habits, physical inactivity, and alcohol consumption[4]. According to a World Health Organization study, 4.9 million people pass away from lung cancer as a result of snuff usage, 2.6 million people die from being overweight, 4.4 million people are dying from excessive cholesterol, and 7.1 million deaths occur from high blood pressure [4].
Traditional examinations in specialized medical facilities were the standard for many years when it came to keeping an eye on heart rhythm, blood pressure, and glucose levels. Because of the rising global population and the increased demand for healthcare resources, there is an increasing burden on medical services. As a result, Healthcare availability in developing countries is already in crisis, and they are seeking to establish a new strategy to distribute medical resources.
In the management of COVID-19 over the world, the terms “Telehealth” and “Telemedicine” are frequently used in public and scholarly research to refer to techniques for providing healthcare remotely [5]. The provision of healthcare remotely via telecommunications technologies is known as telehealth. Telemedicine is the technique of transferring medical information from one location to another using electronic connections in order to enhance a patient’s clinical health state [5].
Telehealth services can help in managing COVID-19 by screening high-risk populations and identifying probable cases, assisting with hospitalized patient care and remotely monitoring people on self-quarantine. In addition, Systems for telehealth can be used to avoid congestion in hospitals and other healthcare facilities. Telehealth can also be utilized to reduce the number of physical clinic visits for patients with chronic illnesses like diabetes or cardiac conditions who are at high risk for COVID-19-related problems [5].
By virtually tying patients and healthcare professionals together around-the-clock, seven days a week, the internet of things provides a new approach. The most crucial factors in a disease diagnosis are vital signs [4]. That is common for Chronic illnesses and Covid-19. Therefore, an inexpensive Healthcare kit on hand would save both time and money, especially who are vulnerable to above-mentioned diseases. Additionally, contactless monitoring and telemedicine capabilities ensure the safety of the both medical staff and patients against Covid-19. Therefore, home monitoring of those indicators will offer a better method for resolving those problems. The smart healthcare kit described in this paper allows both the patient and the doctor to view real-time data at any moment.
2. Literature Review
Vital signs are clinical assessments of a person’s basic body functions that indicate the healthiness of their vital physiological systems. Biological aspects related to this article are mentioned below.
2.1. Vital Signs
Body temperature, Pulse Rate, respiration rate and blood pressure are the vital signs of a human. Medical officials express that vital signs such as blood pressure, temperature, heart rate, oxygen saturation(SpO2), and respiration rate are key indicators of a patient’s present health and must be routinely and precisely recorded [6]. Often, the first evidence of aberrant physiological body changes is seen in the vital signs [6].
2.2 Beats per Minute (BPM)
The number of heart contractions per minute, or heart rate, is a measure of how frequently the heart beats. A pulse is the tactile arterial palpation of the cardiac cycle in medicine (heartbeat). A suitable area to feel the pulse is anywhere on the body where an artery may be squeezed near the skin, such as the neck, wrist, groin, behind the knee, close to the ankle joint, and on the foot [7].
2.3 Oxygen Saturation
The ratio of hemoglobin currently bound to oxygen still unbound is known as oxygen saturation. There are countless numbers of these tiny air sacs in the lungs. They are crucial in bringing carbon dioxide and oxygen molecules into and out of the bloodstream. The body’s tissues receive oxygen when hemoglobin binds to it during circulation.
2.4 Body Temperature
The body uses its temperature as a measure to produce and release heat. The blood vessels on the skin enlarge when someone is overheated to transfer extra heat to the skin [8]. Conversely, a person’s blood vessels narrow when they become too cold, reducing blood flow to the skin and increasing heat production. A person’s average body temperature may be determined via the mouth, ear, underarm, and scrotum.
2.5 Electrocardiogram (ECG)
The electrical activity of the heart during a specific time period is recorded on a graph called an electrocardiogram (ECG) using an electrograph. An ECG is a diagnostic test that examines the cardiac conduction system and provides the doctor with information about the patient’s potential illness processes as well as the health of the patient’s heart.
The heart, a two-stage electrical pump, can have electrodes placed on its surface to assess its electrical activity. The ECG can track the rate and rhythm of the heartbeat as well as give an imprecise indication of blood flow to the cardiac muscle [7]. The PR and QT intervals are the two fundamental intervals of an ECG. The fundamental ECG segments are shown in Figure 1.
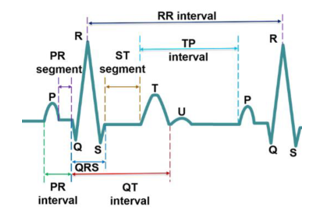
Figure 1. Standard ECG Pulse. Reprinted with permission from [9]
Currently, hospitals use appropriate devices to keep track of their patient’s health. However, doctors must be present in such situations. Researchers came up with various IoT models for healthcare and forecasted various diseases to address this issue. The following are some of the research works done by the authors.
2.6 Wireless Sensor Network-based Smart Healthcare
In the proposed system, a Body Area Network is created by attaching a variety of wireless sensors to the patient’s body to measure important body metrics like temperature, blood pressure, and heart rate. The data is wirelessly gathered and shown on the Patient Bed Monitor (PBM). In addition, the room Server (RS) is connected to it for data archiving and analysis[10].
Three tiers make up the suggested system architecture. Tier-1 comprises wireless sensor nodes fastened to the patient’s temperature and pulse rate to monitor essential body functions. Tier 2 is the intermediate receiving unit that receives the data that has been transmitted. Alert systems and data transmission over larger distances using the right internet connections are the focus of Tier 3[10].
2.7 Raspberry-pi based smart healthcare
Sensors have been connected to the proposed system in appropriate ways. The unit integrates the data from the sensors with the board after receiving it from the sensors[11].
This device connects with the temperature, heart rate, ECG, acceleration, and pressure sensor. In addition, the user’s and doctor’s devices are connected to the internet, and the generated results are shown on a Liquid Crystal Display(LCD) monitor at regular intervals [11].
There are two ways to connect and operate the raspberry device: the first is directly attaching peripherals and the second is connecting the computer after installing the putty program with a IP address, subnet mask, and gateway to that system[11]. If any irregularities in the patient’s health are detected, they will be promptly reported to the authorized or guardian via the Global system for mobile communication (GSM) via the network.
2.8 Arduino-based smart healthcare
The design considered detecting temperature, humidity, and blood pressure. Remote patient monitoring is possible for the aforementioned metrics by medical personnel. The goal of this project was to build a patient health monitoring system that could measure ECG, blood pressure, pulse rate, and temperature [4]. The “ThingView” application displays the ECG, temperature, and pulse rate characteristics visually, and the readings are conveyed to a phone through SMS(Short Message Service).
2.9 GSM-based smart healthcare
Sensors are used to measure vital signs, and Zigbee and GSM are also used to send the parameters wirelessly. An SMS is sent to the doctor in an emergency. In an emergency, a SMS is delivered to the doctor. The patient’s family and the medical community are the key users of the GSM-based health monitoring system. [12]. On the “Thingspeak” website, the results are displayed. The output is produced using the sensor data. An LCD shows the computed heartbeat rate.
2.10 Shortcomings of the available products
The majority of the aforementioned versions do not monitor BPM, SpO2, body temperature, and ECG at the same time. Currently, available items require a significant amount of power to operate. The various models’ precision was insufficient for accurate measurements [13]. Despite the plans being implemented, they were unable to distribute the final products because of the absence of internal resources and a late market launch. These architectural designs may have some privacy issues. People might not want to be completely watched over. They can be concerned that crucial information, including their whereabouts or health status, could be disclosed to other parties with the proper authorization[14].
This project takes an innovative approach to health monitoring by creating a small and affordable system that can measure ECG, blood oxygen, BPM, and body temperature. While similar tools are available, they are frequently pricey and lack the versatility required for daily use. Existing products for measuring ECG, blood oxygen, BPM, and body temperature have limitations that make them unsuitable for usage in the home. For instance, hospital equipment is large and requires qualified personnel to operate. Similarly, most home-based monitoring systems are inaccurate and have a limited feature set. The kit produced in this study, on the other hand, solves these disadvantages by adding modern sensors and microcontrollers which have better accuracy on the body parameters. The kit is intended for home usage, which is both affordable and portable, making it ideal for remote patient monitoring.
3. Product Survey
Several data-gathering approaches were used to get information from the general public and doctors on the smart healthcare kit for home use.
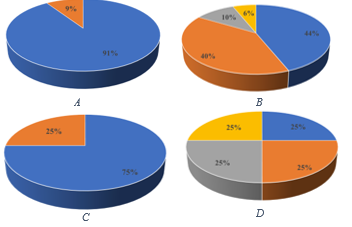
Figure 2. A,B for general people C,D for doctors
3.1 Study for the general public
The authors conducted the research using a Google form. The study enlisted the participation of 120 persons. The experiment lasted for three weeks. Questions that had been asked for the survey are attached below.
- Do you prefer to test your vital signs at home rather than visiting a hospital, and consult a doctor online when you are sick?
- What are your thoughts on the ‘smart-Medicare kit for home usage’?
- Are you willing to monitor patients’ vital signs online, especially in the midst of a pandemic?
- Are you likely to be able to diagnose an illness by taking a patient’s temperature, pulse, SpO2, and ECG?
Figure 2 chart A illustrates that when suffering from a disease, 91% of individuals would prefer to evaluate their vital signs at home than go to a hospital and visit a doctor online. However, 9% would consider going to a hospital physically.
Figure 2 B displays the general public’s perception of the Smart Medicare kit for household use. Almost 45 percent of individuals thought it was a great idea. Approximately 40% voted as ‘Good’. Nevertheless, around 6% think that the idea of a healthcare kit is poor.
3.2 Survey for doctors
If the patient is in critical condition, the system sends an emergency message to a healthcare professional. To calculate vital sign threshold values, a Google form is given to 50 family doctors. Numerous interviews were also done in order to acquire critical information, such as selecting the optimal places of the body to achieve the most exact results. Additionally, the user handbook includes all of the best locations for sensor placement. According to Figure 2, C, almost 75% of doctors are ready to monitor vital signs remotely.
Figure 2, D shows that about a quarter of doctors would be able to detect a basic illness by evaluating the kit’s measurement. Half of those polled believe they can diagnose a sickness to some amount by reading values.
3.3 Survey on Hospitals
Telehealth has been available in the country for a decade, but adoption among the general public has been modest [5]. The Information and Communication Technology Agency of Sri Lanka inaugurated the first IoT project in Sri Lanka in 2015, with 25 state hospitals participating. Following it, various numerous were carried out over the nation [15]. The Ministry of Health has also created mobile applications to help increase Telehealth services in Sri Lanka [5]
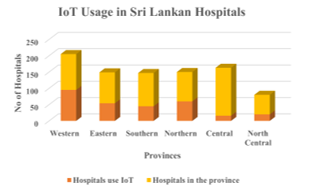
Figure 3. IoT Usage in Sri Lankan Hospitals
An analysis was conducted to determine IoT usage in Sri Lankan hospitals. Personal communications and statistical records were used to obtain data from the Ministry of Health and the Health Informatics Society of Sri Lanka. Figure 3 shows that IoT technology is utilized in practically every province. Medical data management systems, Mhealth apps, and personal health numbers are some examples of IoT applications used in Sri Lankan hospitals. [15]. As a result, hospitals will find it easier to integrate IoT.
According to studies, hospitals may leverage Internet of Things technology to improve the efficiency of healthcare services. IoT technology is transforming the healthcare industry; by incorporating IoT, hospitals may enhance professional efficiency while also offering higher-quality medical treatment. Remote patient monitoring technologies allow medical personnel to minimize fatigue while saving patients the trouble of traveling. This is a huge advantage, particularly for persons with restricted mobility.
4. Flowchart
First and foremost, the Wi-Fi name and Passcode should be supplied in the code. The NodeMCU will attempt to link up to Wi-Fi after connecting the micro-USB to the PC. The Message Queuing Telemetry Transport protocol will be attempted if the device is connected.
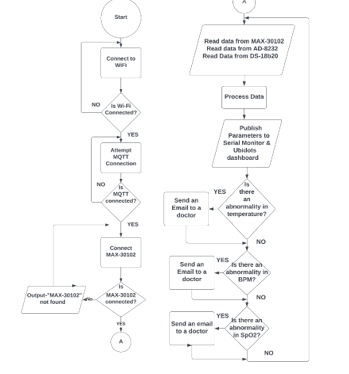
Figure 4. Flowchart of the proposed model
The system will then check the MAX30102 sensor’s availability. If the sensor is present, the kit begins reading data from the MAX-30102, AD-8232, and Temperature sensors. It will then sort out and upload the records to the Serial Monitor and the “Ubidots” cloud platform.
Lastly, any deviations from previously defined threshold values will be detected by the microprocessor. If any of the abnormalities are found, the system will send a message to a doctor based on previously given data, as shown in figure 4.
5. Methodology
The project’s purpose is to create a smart Medicare system that can alert a doctor when a patient is in a severe condition. The project’s aims are to assess a person’s BPM, SpO2, and temperature from home if the person is unwell, to plot an ECG and have it evaluated by a doctor if the person is in a critical condition, and to safeguard both patients and medical staff against Coronavirus.
The esp-8266 offers various functionalities that are extremely useful when working with IoT. The Wi-Fi antenna on the module allows embedded devices to connect to networks and send data. Figure 5 depicts the integration of three sensors. Furthermore, the processer handles fundamental inputs from analog and digital sensors in order to perform significantly more sophisticated calculations. As the “Ubidots” cloud platform is accessed here, the esp-8266 can browse websites written in Hyper Text Markup Language(HTML) or any other development language.
The process began with the purchase of required circuits from shops. Individual codes were then written for each circuit. Following that, all circuitries were rigorously tested for flaws and defects to ensure precise and reliable performance.
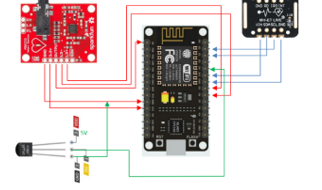
Figure 5. Wiring Diagram
The different circuits were tested and validated before being merged onto a single breadboard, as shown in Figure 5. The codes created for each circuit were concatenated to form a single code. This code was then transferred to the esp-8266 module and thoroughly tested for accuracy and faults. To achieve precise readings, special steps were taken, such as configuring the max30102 sensor to take an average of four data points and setting the AD8232 sensor to record 400 samples per second.
“Ubidots” was chosen as the cloud service for the application. To begin, each sensor’s data was transmitted to the cloud service and reviewed for errors. Second, the sensors were combined, and data was transferred to the cloud. Real-time data was used to discover faults.
A poll of doctors was conducted to determine the temperature, pulse rate, and blood oxygen level thresholds. If the measured values deviate from the threshold value, an email is automatically sent to the relevant family doctor. This was done through the “Ubidots” website. This cloud platform housed medical records. The ECG was slightly off due to network latencies. Hence, the readings from an ECG were exported to Microsoft Excel utilizing the data streamer option. A caretaker then plotted the graph and sent it to a doctor.
The printed circuit board was designed using Autodesk-Eagle. Separate footprints were created for AD-8232 and MAX-3012. The schematic diagram was then created. Third, all of the components were carefully arranged to reduce the length of the copper cables. After the placement, the routing was completed. The trace width was calculated using ‘EE web PCB trace width calculator online tool. Finally, the Gerber files were created and delivered to the manufacturer.
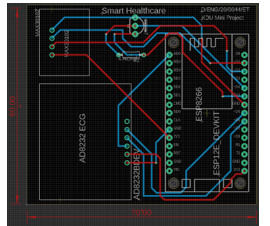
Figure 6. PCB(Printed Circuit Board) Design
The PCB was received and tested for quality after a three-week wait. On the PCB, female header pins were attached, and all sensors were connected to these pins. The sensors’ operation was checked and verified when they were put into the board. A second Vero board was required to fit the Max-30102 sensor. To provide reliable readings, the sensor was positioned on top of the plastic stage and isolated from the other sensors to reduce interference. Since the photoplethysmography(PPG) technique is used in MAX-30102, the sensor was positioned in a dark area to reduce noise and improve measurement accuracy. The configuration was double-checked to confirm that all sensors were working properly.

Figure 7. End Product
Finally, the 3D model was created with AutoCAD. The 3D model was then fed into a laser cutter, which sliced the plastic into the desired shape. Finally, everything was fitted together to make the final product seen in figure 7.
6. Validation of Experimental Results
The complete results of the model implementation are shown below. The model’s output was validated using a temperature and an oximeter. The experiment was carried out on a healthy middle-aged man.
6.1 Body Temperature
Below equation was used to calculate the percentage error. The percentage of body temperature was calculated, as shown in the preceding equation. The experimental value was determined as the average of seven consecutive 30-second observations. The exact value was determined by averaging seven successive “aeg FT4904” thermometer readings taken within 30 seconds.
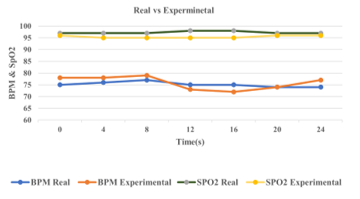
Figure 8. Experimental values from the kit vs real values from the oximeter
6.2 Bpm & SpO2
The real and experimental data were displayed for a time of 24 seconds, as illustrated in figure 8. Real measurements were taken with a “ROHS ABH23” fingertip pulse oximeter. The X-axis depicts the time with four consecutive periods, while the Y-axis reflects BPM and oxygen saturation. There is a slight difference between the real and experimental numbers.
6.3 Electrocardiogram
Figure 9 depicts a tested graph taken from the system. When compared to a standard graph (figure 1), the key segments (PR,ST) and intervals (PR,QT) can be seen. Likewise, it is observed that the experimented data has high accuracy.
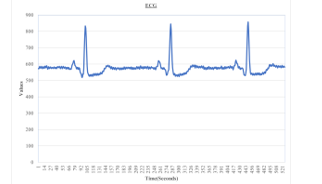
Figure 9. Obtained ECG from the kit
7. Discussion
7.1. Strengths
The model has a number of strengths. The device can assess body temperature, pulse rate, oxygen level, and ECG. (Four in one). As a result, there is no need to acquire a pricey oximeter, thermometer, and ECG machine individually (Cost-effectiveness). If the values differ, it automatically sends a notification to a doctor. Furthermore, it consumes less electricity and can be carried anywhere (Easily equipped). Finally, the model saves time by storing past data.
7.2 Accuracy Improvements
Accuracy enhancement approaches were used to decrease the constraints. For SpO2 and BPM, an average of four data points were collected, while 400 samples were collected every second for ECG and the application of filtering algorithms.
7.3 Issues experienced
The first issue encountered was with the MAX-30102. Pullup resistors were the source of the problem. To make it pull up, they were connected to 1.8v. The microcontrollers, on the other hand, ran on 3.3V. As a result, the three pull-up resistors were taken out with a soldering iron.
The second issue was cloud-based monitoring of the ECG. The real-time graph varied from its conventional graph due to network latency issues. As a response, the values were exported to Microsoft Excel, where the graph was created.
7.4 Price Assessment
The smart healthcare kit was expected to cost 8500.00 LKR in total. In contrast, purchasing the medical equipment individually would cost roughly 50,000 LKR. As a result, there is a large amount of difference that is financially favorable.
7.5 IoT Security Design
Because of the fast development and integration of the Internet of Things in various sectors of our everyday lives, Internet of vulnerabilities has emerged. Cyber-attacks risk the security and privacy of IoT device users. IoT devices don’t have the adequate processing power, energy, storage capacity, and memory[16]. The best method for protecting communications between IoT devices is still being developed.
Security issues are a continual threat to IoT. Because of a large number of Internet-connected IoT devices, the Internet of Vulnerabilities has emerged. “Symantec” reports stated that IoT threats increased 600% in 2017[16]. The criteria for safeguarding IoT systems are authentication, authorization, communication, and device identification. The most secure authentication techniques concentrate on three characteristics: network assumptions, communication sessions, and users.
The “Ubidots” login information is unique to each individual. The password is only known to one person. This is how authentication is protected. The account token, according to the proposed technique, should be sent to someone’s family doctor so that they may verify their live data. As a result, only those people have access to particular information.
| Table 1. The comparison of vital signs to the existing systems |
| Vital signs and systems |
Body Temp. (oC)_ |
BMP (BPM) |
SpO2 (%) |
ECG |
| Proposed kit | 35.005 | 76 | 96 | Similar to fig1 |
| Available system-1 [17] | 28 | 86 | 76 | Vertically shifted |
| Available system-2 [18] | 29.81 | 108 | 63 | unclear |
| Available system-3 [19] | 30.45 | 69 | – | Dissimilar to fig1 |
| Table 2. Percentage errors of the existing systems |
| Percentage error of Body Temp(%) | Percentage error of BPM(%) | Percentage error of SpO2(%) | |
| Proposed Kit | 5.6 | 5.2 | 1.0 |
| system-1 | 32.21 | 16.27 | 27.6 |
| system-2 | 24.11 | 33.33 | 53.9 |
| system-3 | 21.5 | 4.3 | – |
To assess the efficacy of our IoT-based healthcare equipment, the accuracy of industry benchmarks was compared. As presented in table 1 BPM, SpO2, ECG, and body temperature results were compared to the previous similar studies.
According to the findings in table 2, the proposed healthcare kit had fewer percentage errors. The percentage error was calculated according to equation 1. Actual values were considered as 37oC, 72 and 97% for body temperature, BPM and SpO2 respectively which are general truths. When compared to currently commercialized products, our healthcare kit outperformed the above systems in terms of body temperature and SpO2 accuracy. The ECG of the available system 1 was shifted vertically. Therefore, the vertical measurements were affected. ECG of the available system 2 was unclear and the diagnosis procedure is quite hard. By mitigating the drawback of each existing product mentioned in 2.10, these findings indicate that our healthcare kit has the potential to deliver precise and accurate vital sign measurements for home users.
8. Future Directions and Concluding Remarks
Future enhancements include adding blood pressure equipment to the smart healthcare unit, developing a model utilizing Machine Learning Algorithms to assess ECG data, and sending an automated message to an ambulance service. Furthermore, security enhancements should be implemented to tighten privacy and reduce cyber-attacks.
Artificial Intelligence (AI) in healthcare combines computation with the viewpoints of doctors to build better healthcare technologies. Using NLP, knowledge representation, automated reasoning, and machine learning, AI attempts to make computers more practical and intelligent. Understanding patient health status by a pre-trained model from symptoms could be a future advancement.
Some of the product’s primary features include keeping a patient’s medical records, alerting a doctor in an urgent emergency, four in one, and many more. The combination of these features makes it a great tool for both individuals looking to monitor their health from the comfort of their own homes and healthcare professionals looking for an accurate solution for remote patient monitoring.
The goal of this research is to develop an IoT-based smart healthcare kit for people suffering from Covid and Chronic diseases. The project was completed and tested with people successfully. We’d like to thank everyone who took the time to fill out the survey. The information obtained was useful in determining a continuing problem and a long-term remedy.
- Y. Kodithuwakku, A.D. Sandanayake, C. Bandara, V. Logeeshan, “IoT Based Healthcare Kit for Domestic Usage,” 2022 IEEE World AI IoT Congress, AIIoT 2022, 760–765, 2022, doi:10.1109/AIIoT54504.2022.9817235.
- A.K. Singh, A. Misra, “Impact of COVID-19 and comorbidities on health and economics: Focus on developing countries and India,” Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 14(6), 1625–1630, 2020, doi:10.1016/j.dsx.2020.08.032.
- E. Workie, J. Mackolil, J. Nyika, S. Ramadas, “Deciphering the impact of COVID-19 pandemic on food security, agriculture, and livelihoods: A review of the evidence from developing countries,” Current Research in Environmental Sustainability, 2, 100014, 2020, doi:10.1016/j.crsust.2020.100014.
- K. Latha, G. Sravanth, N.V.P. Kumar, …, “An IoT based patient monitoring system using arduino uno,” … Research Journal of …, 2020.
- G.G. Kulatunga, R. Hewapathirana, R.B. Marasinghe, V.H.W. Dissanayake, “A review of Telehealth practices in Sri Lanka in the context of the COVID-19 pandemic,” Sri Lanka Journal of Bio-Medical Informatics, 11(1), 8, 2020, doi:10.4038/sljbmi.v11i1.8090.
- W.Q. Mok, W. Wang, S.Y. Liaw, “Vital signs monitoring to detect patient deterioration: An integrative literature review,” International Journal of Nursing Practice, 21(S2), 91–98, 2015, doi:10.1111/ijn.12329.
- R. Mahajan, D. Bansal, “Identification of heart beat abnormality using heart rate and power spectral analysis of ECG,” International Conference on Soft Computing Techniques and Implementations, ICSCTI 2015, 131–135, 2016, doi:10.1109/ICSCTI.2015.7489555.
- M.U.H. Al Rasyid, B.H. Lee, A. Sudarsono, “Wireless body area network for monitoring body temperature, heart beat and oxygen in blood,” 2015 International Seminar on Intelligent Technology and Its Applications, ISITIA 2015 – Proceeding, 95–98, 2015, doi:10.1109/ISITIA.2015.7219960.
- L. Xie, Z. Li, Y. Zhou, Y. He, J. Zhu, “Computational diagnostic techniques for electrocardiogram signal analysis,” Sensors (Switzerland), 20(21), 1–32, 2020, doi:10.3390/s20216318.
- U. Gogate, J.W. Bakal, “Smart Healthcare Monitoring System based on Wireless Sensor Networks,” International Conference on Computing, Analytics and Security Trends, CAST 2016, 594–599, 2017, doi:10.1109/CAST.2016.7915037.
- N. Arunpradeep, G. Niranjana, G. Suseela, “Smart healthcare monitoring system using iot,” International Journal of Advanced Science and Technology, 29(6), 2788–2796, 2020, doi:10.22214/ijraset.2020.5101.
- K. Aziz, S. Tarapiah, S.H. Ismail, S. Atalla, “Smart real-time healthcare monitoring and tracking system using GSM/GPS technologies,” 2016 3rd MEC International Conference on Big Data and Smart City, ICBDSC 2016, 357–363, 2016, doi:10.1109/ICBDSC.2016.7460394.
- A. Rahaman, M.M. Islam, M.R. Islam, M.S. Sadi, S. Nooruddin, “Developing iot based smart health monitoring systems: A review,” Revue d’Intelligence Artificielle, 33(6), 435–440, 2019, doi:10.18280/ria.330605.
- D. Ding, M. Conti, A. Solanas, “A smart health application and its related privacy issues,” Proceedings of the 2016 Smart City Security and Privacy Workshop, SCSP-W 2016, 11–15, 2016, doi:10.1109/SCSPW.2016.7509558.
- R. Rajmohan, P.D.D.M.G.M. Johar, “Adoption of the Internet of Things in the Healthcare Services of Sri Lanka,” International Journal of Recent Technology and Engineering (IJRTE), 9(1), 1095–1104, 2020, doi:10.35940/ijrte.a2260.059120.
- M.A. Obaidat, S. Obeidat, J. Holst, A. Al Hayajneh, J. Brown, “A comprehensive and systematic survey on the internet of things: Security and privacy challenges, security frameworks, enabling technologies, threats, vulnerabilities and countermeasures,” Computers, 9(2), 2020, doi:10.3390/computers9020044.
- A.D. Acharya, S.N. Patil, “IoT based Health Care Monitoring Kit,” Proceedings of the 4th International Conference on Computing Methodologies and Communication, ICCMC 2020, (Iccmc), 363–368, 2020, doi:10.1109/ICCMC48092.2020.ICCMC-00068.
- M.R.R. Akash, Yousuf, K. Shikder, “IoT Based Real Time Health Monitoring System,” Proceedings of International Conference on Research, Innovation, Knowledge Management and Technology Application for Business Sustainability, INBUSH 2020, 167–171, 2020, doi:10.1109/INBUSH46973.2020.9392163.
- M.R. Ruman, A. Barua, W. Rahman, K.R. Jahan, M. Jamil Roni, M.F. Rahman, “IoT Based Emergency Health Monitoring System,” 2020 International Conference on Industry 4.0 Technology, I4Tech 2020, 159–162, 2020, doi:10.1109/I4Tech48345.2020.9102647.
