Quality Function Deployment: Comprehensive Framework for Patient Satisfaction in Private Hospitals
Volume 6, Issue 1, Page No 1440-1449, 2021
Author’s Name: Mohammad Kanana), Siraj Essemmar
View Affiliations
Industrial engineering Department, College of Engineering, University of Business and Technology, Jeddah, 21448, Kingdom of Saudi Arabia
a)Author to whom correspondence should be addressed. E-mail: m.kanan@ubt.edu.sa
Adv. Sci. Technol. Eng. Syst. J. 6(1), 1440-1449 (2021); ![]() DOI: 10.25046/aj0601163
DOI: 10.25046/aj0601163
Keywords: Quality function deployment, House of quality, Healthcare sector, Voice of the customer, Quality of service, Saudi Arabia
Export Citations
This paper addresses the quality of private healthcare services in the western region of the Kingdom of Saudi Arabia (KSA) and provides a comprehensive analysis of the customer requirement to improve the quality of these services. The study begins by reviewing literature on the subject of quality in general and then in terms of the service and healthcare sectors. To assess the healthcare system, the paper then presents the literature on accreditation, which is a tool for healthcare quality assessment. Past studies in healthcare are also reviewed. The voice of the customer (VOC) is an essential factor in this study, so the quality function deployment (QFD) tool was implemented to satisfy the customer requirements and achieve the purpose of the study. A customer focus group was used to determine the VOC, and a survey of 300 samples was conducted to assess the importance of each requirement. The study implemented four houses, which represent the four phases of a comprehensive QFD. According to QFD analysis the results show that there are two main factors that affect the private healthcare system in the (KSA). The first factor deals with management issues, while the second one relates to the recording and flow of information. The study suggests several ways to improve the management and information issues of the healthcare system in (KSA).
Received: 08 December 2020, Accepted: 19 February 2021, Published Online: 28 February 2021
1. Introduction
Due to globalization and the rapid changes in various industries, improvement in the quality of the healthcare sector has been relatively slow. As such, the governments need to give serious attention to this sector, which delivers one of society’s basic needs. The population of the Kingdom of Saudi Arabia (KSA) is approximately 34 million, with an annual population growth rate of 2.52% (General Authority of Statistics). According to United Nations projections, by 2025 the population of KSA will be approximately 39.8 million [1]. Hence, KSA’s 2030 vision includes several initiatives to improve its healthcare services. Currently, there are three medical sectors in KSA: the government agencies sector, the public healthcare sector, and the private healthcare sector. The government agencies sector makes up 17.7% of total healthcare services, and provides healthcare services to specific government employees and families through specialist hospitals and research centers, National Guard health affairs, security forces medical services, Royal Commission health services, army medical services, and the Ministry of Education hospital [2]. The public healthcare sector makes up 60.2% of total healthcare services, which are provided by the Ministry of Health (MOH). The private sector makes up 22.1% of total healthcare services [2]. The MOH plans to transfer 295 hospitals and 2,259 health centers to the private sector by 2030 [1]. It also revealed that, out of 2,390 healthcare centers in KSA, only 55 have attained the standards of the Saudi Central Board for Accreditation of Healthcare Institute (CBAHI) (CBAHI, 2013). The governments needs to establish a new system, method, and measurement of quality that will enhance performance, reduce costs, and eliminate waste. This study aims to improve the quality of private healthcare services in the western region of KSA. The study focuses on patients as a major stakeholder in these services. Although the suggestions are related to the structure and process of healthcare systems, they also affect the outcomes in the healthcare service framework. To achieve this aim, it is essential to evaluate current services and the performance of competitors, for which the quality function deployment (QFD) tool will be used.
2. Literature review
The quality definitions is highly debated in the associated literature. However, a challenge arises due to the difference in perspectives of different types of products, which range from goods and services to software [3].
2.1. Quality review
In terms of goods, there are multiple definitions of quality. In 1984, Garvin dealt with quality by categorizing past definitions into five approaches—value based, product based, user based, transcendent, and manufacturing based—and separating the basic elements of product quality into eight dimensions [4]. Also, Garvin studied the relationship between quality and other terms such as marketing, price, and cost. He discussed four types of costs which are: appraisal cost, external and internal failures, and prevention cost [4]. Feigenbaum coined the term cost of quality in a 1956 which include the four types of cost [5]. Juran defined quality as “fitness for use” and argued that an analogy can be made between financial management and quality management, establishing a tripartite approach of quality planning, quality control, and quality improvement [3]. Japanese philosophy defines quality as having no defects, being done right the first time. Reinforcing the latter definition, Crosby defined quality as “conformance to requirements or specifications” [6]. Deming’s definition of quality is slightly more expansive: “Quality is a predictable degree of uniformity and dependability, at low cost and suited to the market”. Deming also identified 14 areas of quality management that support and improve an organization’s performance [7].
Quality of service, however, differs from the quality of tangible goods. Parasuraman and Grönroos defined quality of service as the perceptions of consumers that are associated with their expectations of the service and the received service [8]. Parasuraman and Grönroos’s definition established quality as the gap between customers and managers. They identified five types of gap—knowledge, standards, delivery, communications, and expected service/perceived service—and ten dimensions of service quality, which they called SERVQUAL. Although SERVQUAL is one of the most common models used in the literature for services similar to healthcare, such as tourism, hospitality, marketing, and banking, it needs to be modified to fit the context [9]. Cronin and Taylor rejected this method of gaps/score measurement, instead measuring service quality using a tool called SERVPERF, which depends only on performance [9].
Many recently developed products are software based, and software has become a significant factor in quality of life. Both goods and services depend on software. As such, the need to understand, control, and design high-quality software has become important [10]. Managers generally focus on improvement, so researchers have designed tools and instruments to measure and improve quality in any field. In the United States manufacturing industry during the 1980s, quality was transformed from small-q to big-Q. This change, established by Juran, highlighted the difference between focusing on reworking existing conditions in a limited capacity (small q), which often neglected other factors like resources and management, and managing quality in all aspects of business (big Q). This concept later became known as total quality management (TQM) [11]. TQM is an organized approach to achieving customer satisfaction using several techniques, tools, and systems through continuous improvement of a process [12]. In 1987, the Malcolm Baldrige National Quality Award was established and the Lean Six Sigma was revealed by Motorola. The Lean Six Sigma is a model that focuses on the variations of products to reduce the chance of defects to less than 3.4 per million. Its methodology follows five stages: definition, measurement, analysis, improvement, and control (DMAIC) [13].
2.2. Quality in the service industry
Literature has identified three main economic sectors: the primary sector, the secondary sector, and the tertiary sector. The primary sector deals with the extraction of natural resources through farming and mining, while the secondary sector transforms these raw materials into tangible goods. The tertiary sector focuses on the production of services rather than goods, and has a significant effect on gross domestic product (GDP). It also greatly impacts everyday life in areas such as education, healthcare, and transportation.
According to the Oxford English Dictionary, a service is “a system supplying a public need such as transport, communications, or utilities (electricity and water)”. The Business Dictionary defines service as “a valuable action, deed, or effort performed to satisfy a need or to fulfill a demand”. Service involves all aspects of modern life—it is the several processes that deliver benefits to customers. The nature of service is more complex than that of tangible goods, and the problems of the service sector are related to the characteristics of different services, which can be classified into three main categories: intangibility—a service is performed, rather than being an object, so it cannot be measured in advance to assure the quality—heterogeneity—a service depends on the performance of staff, so it differs from one provider to another—and inseparability—the delivery of a service depends on the interaction between a customer, a provider, and their environment [6]. One of the limitations of a service is that a customer cannot evaluate its quality until they have experienced it, a limitation that Phillip Nelson highlighted when he distinguished between “search” and “experience”. In search, quality can be determined before purchase, but in experience it can only be known after purchase and use [4]. The limited knowledge of the customer in the healthcare process makes it harder to judge the quality of healthcare service.
2.3. The definition of healthcare quality
Healthcare is a complex service system; according to Donabadian’s framework, the healthcare system consists of three main categories: structures, processes, and outcomes. While structures relate to facilities, equipment, layout, and physicians, a process is any interaction between the customer and the healthcare structure. Outcomes are the consequences of the healthcare service [14]. Overall, the healthcare system provides benefits to several stakeholders, including patients, attendants (relatives, friends), physicians, nurses, insurance companies, and the government.
Scholars and researchers have provided different definitions of high-quality healthcare. Ovretveint defined it as “fully meeting the needs of those who need the services most, at the lowest cost to the organization, within the limits and directive set by higher authorities and purchases” [2]. Campbell, Roland, and Buetow (2000) categorized high-quality healthcare into two types: individual patient care and population care. Individual patient care is defined as “whether individuals can access the health structures and processes of care which they need and whether the care received is effective”. Population care is “the ability to access effective care on an efficient and equitable basis for the optimization of health benefit/well-being for the whole population”. Deepti Singh and Kavaldeep Dixit argued that the satisfaction of the patient will be achieved by improving the delivery of health care service, considering patients’ needs, and reacting with their annotation [15]. So, the involvement of patients and shear their experience with healthcare professionals is a critical factor that will impact the quality improvement process [16].
2.4. Healthcare quality standards
An effective factor in assessing and improving quality is accreditation—a framework to help and improve the quality of healthcare by fulfilling the standards of an external independent accreditation body [17]. Standards are a measure of excellence that indicate key functions, processes, structures, and activities. In healthcare facilities, it is a requirement to assure the provision of safe and high-quality care [18] . Although standards are the tools and requirements of accreditation, they also help an organization improve the quality of its services [19] . Araujo, C. A., Siqueira, M. M., & Malik, A. M reviewed 37 studies about the impact of accreditation on the healthcare quality and they concluded that the accreditation effects on healthcare quality indicators are mostly positive [20].
2.5. The Saudi Central Board for Accreditation of Healthcare Institutions (CBAHI)
The CBAHI is a non-profit governmental organization authorized to give accreditation to healthcare centers in KSA. It aims to continually improve healthcare services in terms of quality and safety, and seeks to achieve this by supporting healthcare facilities in following the established standards. The organization was itself accredited by the International Society for Quality in Healthcare (ISQua), making it one of the few healthcare accreditation organizations around the globe. In the CBAHI’s third edition standards manual, there are 23 chapters explaining the functions and key services that must be provided to obtain accreditation, such as leadership, nursing care, quality management, patient safety, operating rooms, facility management, safety, and emergency care [18].
2.6. Healthcare quality studies
Several relevant case studies have been conducted in healthcare literature. Due to the difficulties associated with measuring quality in healthcare sectors, different models were employed based on the tools or methods used. One of the most popular models used in the healthcare sector is SERVQUAL, and although some researchers were committed to Parasuraman’s dimensions, a modified SERVQUAL model was needed in some case studies. For example, authors studied the relationship between patient satisfaction, service quality, and word of mouth (WOM), concluding that the main dimension of service quality that affects WOM is empathy, and that some dimensions, such as assurance, responsiveness, and tangibility, have an indirect effect on patient satisfaction [8]. Later, authors applied a new scale to measure SERVQUAL gaps in Malaysian private healthcare services [21]. Padma, Rajendran, and Sai (2009) found that the dimensions of SERVQUAL are not sufficient to reflect actual quality level, so they adapted dimensions from the Malcolm Baldrige National Quality Award (MBNQA, 2007) and Joint Commission International framework (JCI, 2007) and modified dimensions in [9].
Some researchers have used another model, the plan–do–study–act (PDSA) model, which is a tool for quality improvement developed by Shewhart and Deming. The model consists of four stages: the planning stage, which identifies the improvement of the process; the doing stage, which deals with testing the improvement; the studying stage, which examines the success of the improvement; and the acting stage, in which a new cycle is initiated by the identification of further possible adaptations [22]. Authors reviewed 73 articles related to healthcare and found that more than 60% of the articles fulfilled PDSA criteria and information. Based on their findings, the benefits of the PDSA can be maximized by starting the cycle on a small scale and following an iterative approach [22].
Other researchers have expanded the concept of healthcare quality through the use of TQM. Dilber, Bayyurt, Zaim, and Tarim (2005), for example, identified the critical factors of TQM in the healthcare sector—process management, the role of top management, employee relations, and data reporting—and measured the impact of these critical factors on business performance in Turkish hospitals [7]. Some authors also integrated TQM with business process re-engineering (BPR), which is a fundamental and radical redesign and rethinking of business processes to create significant improvements in performance [3].
2.7. Quality function deployment (QFD)
One of the main critical factors in TQM is the voice of the customer (VOC). There are several ways to study the VOC, one of the most popular tools is the quality function deployment (QFD).
In 1972, authors published a paper about quality deployment. This, along with Nishimura’s paper, was the route of the new concept of QFD to the west. Authors then established a way to convey customer requirements from the design stage to the operation stage, called quality function deployment (hinshitsu kino tenkai). Finally, in 1978, a book titled Deployment of the Quality Function, which discussed the Japanese experience of QFD [23].
QFD is a tool for transforming customer requirements into design with a satisfying level of quality assurance, and can create novel solutions [23]. It can, however, be difficult to apply, as it is loosely defined and can therefore be more of an art than a science [23].
The primary fields into which QFD was introduced were quality management systems, customer needs, product development, and analysis. It was later extended to other fields, such as construction, costing, education, decision making, software, and services. QFD can be used in any field, without boundaries [23, 24].
House of quality (HOQ) is the basic design tool of QFD. It started in 1972 in Mitsubishi’s Kobe shipyard, and was then implemented by Toyota in different ways. HOQ is a conceptual map that provides the means for inter-functional planning and communication. The main principle of HOQ is to satisfy customer needs by learning from customer experiences [25]. QFD uses several iterations of HOQ to translate customer needs into detailed functional characteristics, and these iterations (houses) require a high level of cooperation between cross-functional teams [26]. Jaiswal (2012) defined these iterations as product planning, product design, process planning, and process control [27]. The authors explained that implementations in QFD often need several HOQ repetitions to obtain a satisfactory result, but organizations usually only get through the first house of QFD [27].
Generally, there are two main phases in each house or iteration; the first phase deals with the quality plan, answering the “What” questions, while the second phase is related to quality design, answering the “How” questions [28]. “What” questions appear in the HOQ conceptual map (see Figure 1) as room (1), containing customer requirements or preferences. Beside it, the priorities being assigned based on customer preferences. The engineering characteristics are generated and entered in room (3). The biggest room, constructed between the “How” and “What” questions, is room (4), the relationship matrix, which indicates how much the “How” and “What” relate to or affect each other. Rooms (5) and (6), respectively, represent the benchmark for customer satisfaction and engineering characteristics correlating to benchmarks. Room (7) is located at the bottom of the house and includes the targets for a new product or service. The final part of the house is a coupling matrix, which appears as room (8), the roof. This is used to show the relationship between one engineering characteristic and another [29].
 Figure 1: House of quality model [33]
Figure 1: House of quality model [33]
3. Study Execution
This study aims to provide appropriate suggestions for improving service quality and satisfying customer needs in the private healthcare sector in KSA. As the VOC is the core of this paper, the QFD was used.
3.1. Methodology
To determine customer requirements (the VOC), a focus group session was held with customers then the survey was conducted to measure the importance of customer requirements. The results were analyzed and based on the analysis, the HOQ was established to generate the engineering characteristics. A scale of 0, 1, 3, and 5 points was used in the relationship matrix, as put forward in [30]. To achieve comprehensive analysis, benchmarking was performed in each phase and the public and other government agencies were seen as competitors.
3.2. Gathering the VOC
Customers were gathered in Jeddah from different ages and perspectives to determine the most important needs based on their experience with different private hospitals. The sessions discussed Cooperation of medical staff, Waiting time, Ease of procedures, And Cost of medical care among others. As shown in table 1. The sessions took more than 30 hours spanning five days. Doctors and experts were also consulted.
Table 1: Importance of customer requirements
| n | Customer requirement | Weight | Percentage | Customer importance |
| 1 | Waiting time | 2643 | 11.26% | 9 |
| 2 | Availability of appointments | 2776 | 11.82% | 9 |
| 3 | Cooperation of medical staff | 2893 | 12.32% | 10 |
| 4 | Cooperation of administrative staff | 1973 | 8.40% | 7 |
| 5 | Quality of facilities | 2256 | 9.61% | 8 |
| 6 | Reputation of the hospital | 2296 | 9.78% | 8 |
| 7 | After-service communication | 1112 | 4.74% | 4 |
| 8 | Ease of procedures | 2032 | 8.65% | 7 |
| 9 | Software application | 1108 | 4.72% | 4 |
| 10 | Calling method in the waiting room | 1068 | 4.55% | 4 |
| 11 | Access to medical records | 1165 | 4.96% | 4 |
| 12 | Cost of medical care | 2156 | 9.18% | 7 |
Table 2: Engineering characteristics for product planning
| n | Engineering characteristic | Explanation |
| 1 | Scheduling | Scheduling of appointments/employees |
| 2 | Training and consultation | Periodic training in communication and empathy |
| 3 | Ergonomics | Making workplaces suitable for people |
| 4 | Facility layout | Arrangement and state of the facility |
| 5 | Optimizing the number of patients and resources | Eliminating waste and regulating the number of patients for each doctor |
| 6 | Motivating employees | Encouraging doctors and other staff to be kind and inspiring them to perfection |
| 7 | Accreditation | Achieving the specifications and standards of the CBAHI |
| 8 | Information systems | Information flow within the hospital and other healthcare centers |
| 9 | Communicating with patients | Any process of communication with patients |
| 10 | Encouraging patients to take out insurance | Convincing and influencing patients to take out insurance |
| 11 | Making the app easy to use | Simplifying the app and making it user friendly |
The results from the focus group and consultation sessions revealed that there are 12 requirements to be considered. The 300-sample size survey was conducted to know the priority of each requirement. Using the ranks obtained in the survey questions, the highest customer preference was multiplied by 12, the second highest by 11, the third highest by 10, and so on, to balance the weight of importance for each customer requirement. To modify the scale of customer requirements to between 1 and 10, the weight percentage was multiplied by 80. The outcomes are shown in Table I.
3.3. Product planning
The first house was built based on the survey analysis. After looking at the VOC in the first two rooms, the third room was constructed by listening to the voice of the engineers on how to satisfy the customer requirements, So the engineers studied all requirements and suggested the solution (characteristic) that will affect them. Table 2 shows out the engineering characteristic – representing the suggested solution – and a brief description of each one.
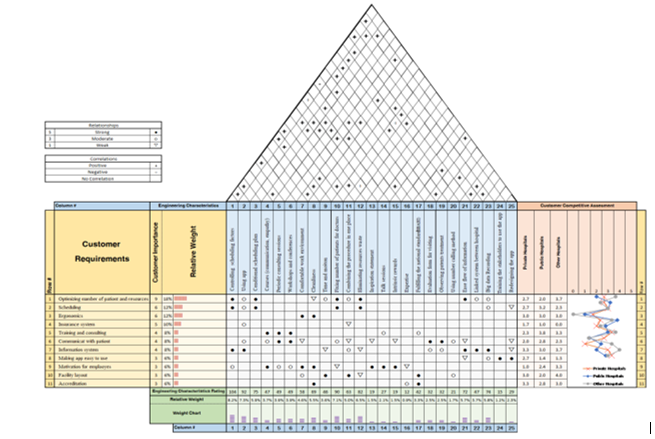
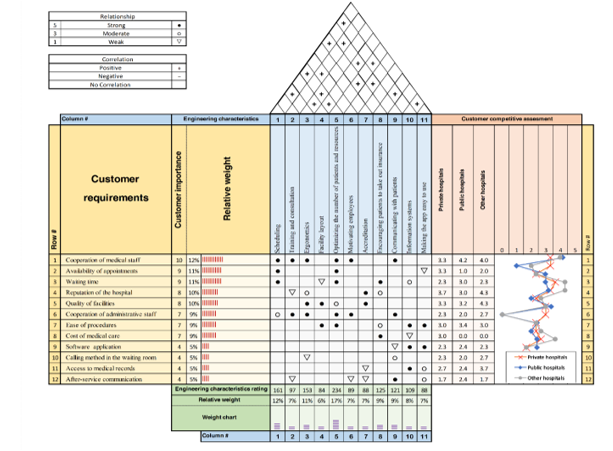 Figure 2: Engineering characteristics details
Figure 2: Engineering characteristics details
The relationship between customer requirements and engineering characteristics was then determined in the correlation matrix. Negative and positive signs were also used to determine the correlation between each engineering characteristic. Finally, the relative weight for each customer requirement and engineering characteristic was calculated. The results of the first phase identified 11 engineering characteristics and the details were represented in Figure 2.
The highest value represents the “optimizing number of patients and resources”. So, focusing on the “optimizing the number of patients and resources” will satisfied customer requirements by 19%. Focusing on a hospital’s internal environment is one of the most valued outcomes, appearing with a high value in both the ergonomics and facility layout characteristics. In relation to encouraging patients to take out insurance, Saudi labor law requires private companies to pay the health coverage costs (insurance) for all employees [31], but other employees should be encouraged to take out their own insurance. As such, encouraging patients to take out insurance is an engineering characteristic that can help minimize the cost of medical care.
3.4. Product design
The engineering characteristics of the previous phase were added as the requirements in this phase, and a new set of engineering characteristics was generated, as shown in Table 3. To satisfy the requirements, controlling scheduling factors should be prioritized, as it has the highest impact on the requirements (see Figure 3). Fixing the number of patients for each doctor is shown to be important, as it reduces physician burnout, which would otherwise affect the healthcare system [32].
Table 3. Engineering characteristics for product design
| n | Engineering characteristic | Explanation |
| 1 | Controlling scheduling factors | Identifying and limiting the factors that can affect scheduling, such as breaks, number of physicians, and appointment duration |
| 2 | Using the app | Involving the app in the communication and information recording process |
| 3 | Conditional scheduling plans | Backup plans for scheduling |
| 4 | Courses (communication, empathy) | Guidelines and seminars on communication and empathy |
| 5 | Periodic consultation sessions | Regular therapy consultations to deal with stress and burnout |
| 6 | Workshops and conferences | Lectures and motivational events |
| 7 | Comfortable work environment | Making workplace conditions more comfortable |
| 8 | Cleanliness | The state of the facility |
| 9 | Time and motion studies | Studying the time of each process and the movement effort required |
| 10 | Fixing the number of patients for each doctor | Regulating the number of patients each physician treats in a day |
| 11 | Combining a procedure in one place | Gathering the process for ease |
| 12 | Eliminating resource waste | Reducing wasted time, effort and equipment |
| 13 | Inspiring statements | Statements aimed to motivate employees |
| 14 | Talks | Inviting motivational speakers |
| 15 | Intrinsic rewards | Non-material incentives for employees |
| 16 | Expertise | Hiring a specialist physician |
| 17 | Fulfilling the national standards (CBAHI) | Achieving the CBAHI standards |
| 18 | Evaluation forms for visitors | Assessment from patients receiving services |
| 19 | Observing patient treatments | Observing the state of patients after discharge |
| 20 | Using a number calling method | Using a numbered queuing technique |
| 21 | Ease of information flow | Ensuring information travels between departments easily |
| 22 | Linked system between hospitals | Integrating a database between all hospitals |
| 23 | Big-data recording | Using big-data principles to record all information |
| 24 | Training stakeholders to use the app | Training patients and staff to use the app properly and effectively |
| 25 | Redesigning the app | Redesigning the interface and functionality of the app |
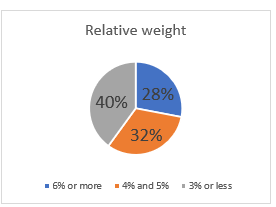 Figure 4: Relative weight of engineering characteristics for product design
Figure 4: Relative weight of engineering characteristics for product design
3.5. Process planning
According to authors, only the most important characteristics from each phase should be moved to the next phase. Therefore, the Pareto method was used to focus on the characteristics that were found to have the greatest impact on the requirements. The impact of each characteristic was detailed on table 4. From that table and following Pareto principal, 28% of these characteristics were moved to the next phase as requirements. (see Figure 4)
Table 4: Engineering characteristics: Contribution to product design
| Engineering characteristics | Relative weight | Cumulative | Relative weight after rounding |
| Controlling scheduling factors | 8.22% | 8.2% | 8% |
| Using the app | 7.27% | 15.5% | 7% |
| Fixing the number of patients for each doctor | 7.11% | 22.6% | 7% |
| Eliminating resource waste | 6.48% | 29.1% | 6% |
| Conditional scheduling plans | 5.93% | 35.0% | 6% |
| Big-data recording | 5.85% | 40.9% | 6% |
| Ease of information flow | 5.69% | 46.6% | 6% |
| Cleanliness | 5.45% | 52.0% | 5% |
| Combining a procedure in one place | 4.98% | 57.0% | 5% |
| Comfortable work environment | 4.58% | 61.6% | 5% |
| Periodic consultation sessions | 3.87% | 65.5% | 4% |
| Workshops and conferences | 3.87% | 69.3% | 4% |
| Courses (communication, empathy) | 3.72% | 73.0% | 4% |
| Linked systems between hospital | 3.72% | 76.8% | 4% |
| Time and motion | 3.64% | 80.4% | 4% |
| Fulfilling the national standards (CBAHI) | 3.32% | 83.7% | 3% |
| Evaluation forms for visitors | 2.53% | 86.2% | 3% |
| Observing patient treatments | 2.53% | 88.8% | 3% |
| Redesigning the app | 2.29% | 91.1% | 2% |
| Talks | 2.13% | 93.2% | 2% |
| Using a number calling method | 1.66% | 94.9% | 2% |
| Inspiring statements | 1.50% | 96.4% | 2% |
| Intrinsic rewards | 1.50% | 97.9% | 2% |
| Training the stakeholders to use the app | 1.19% | 99.1% | 1% |
| Expertise | 0.95% | 100.0% | 1% |
Table 5: Engineering characteristics for process planning
| n | Engineering characteristics | Explanation |
| 1 | Forecasting the number of patients | Predicting the daily demand of patients |
| 2 | Deposit fees for appointments | Fees paid to confirm the appointment and deducted from medical costs |
| 3 | Periodic breaks | Giving breaks to staff during working hours |
| 4 | Providing an internet connection | Availability of an internet connection within hospital facilities |
| 5 | Self-service machines | Machines for patients to facilitate procedures |
| 6 | Research on human subjects | Conducting studies in anthropological fields |
| 7 | Lean Six Sigma tools | Using Six Sigma principles and tools |
| 8 | Establishing a big-data department | Forming a new department for big-data collection and analysis |
| 9 | Standard platforms | Unified platforms containing medical records and other information |
| 10 | Computerized communication between departments | Eliminating all paperwork and replacing it with electronic communication |
| 11 | Replacement people for every job | Assigning employees to cover the absences of others |
From the requirements, 11 engineering characteristics were considered as solutions. The descriptions of each characteristic are summarized in Table 5.
Resource waste caused by the transfer of information between departments has an impact on several factors (See Figure 5).
Computerized communication between departments uses fewer resources, such as paper and time. Moreover, its application enhances patient service and helps in the improvement of scheduling, data recording, and the flow of information. One of the other conclusions of this phase is that the impact of forecasting the number of patients will help reduce the chance of physician burnout, hence improving the quality of patient care [32].
3.6. Process control
The final technical solutions were conducted in this phase. The engineering characteristics of this phase (see Table 6) can be considered the main factors in achieving the customer requirements in the first house.
This phase proved that information could affect quality in healthcare and showed that information has the highest rating in the engineering characteristics of gathering information and contracting IT companies (See Figure 6). The contracted IT company has the responsibility of analyzing and recording information, while leadership faces a challenge in collecting the correct information from various departments. Efficient record keeping and documentation can be difficult [17].
The involvement of IT companies would require time and money, but would help improve information systems by contracting expertise or hiring a specialized employee. The assignment of surveying responsibility to a quality department would also improve quality. This department should be given an extensive training program before its staff are considered qualified to conduct surveys [17].
4. Result and discussion
To summarize the analysis of the QFD and satisfy the customer requirements, two main factors should be taken into consideration. The first factor is management, which was revealed in the first phase to consist of optimizing the number of patients, scheduling, and accreditation. This was expanded in the second phase to controlling scheduling factors, conditional scheduling plans, fixing the number of patients, and fulfilling standards.
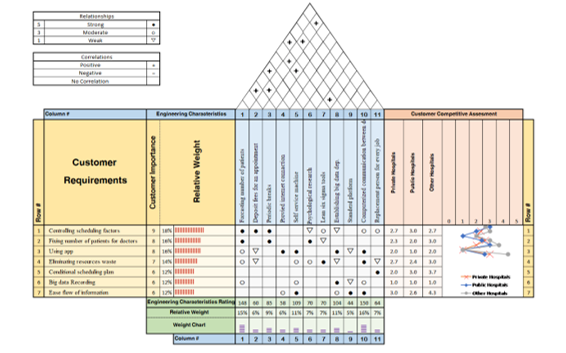 Figure 5: Process planning
Figure 5: Process planning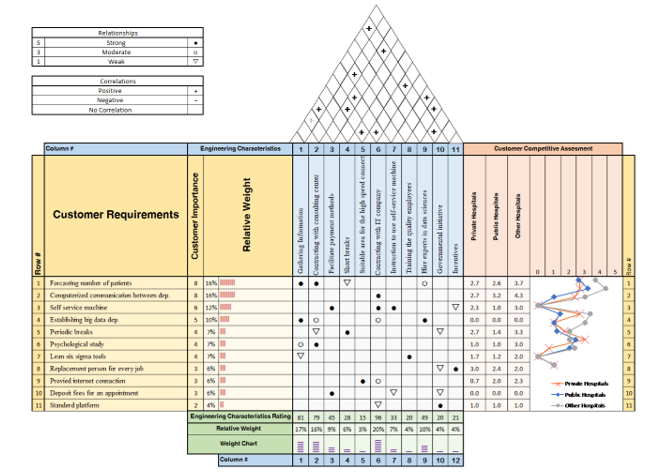 Figure 6. Process control
Figure 6. Process control
This consideration has some contributions to third and fourth phases, such as forecasting the number of patients and contracting a consulting center. The second factor is information, which begins in the first phase with an information system and develops into ease of information flow, big-data recording, and linked systems between hospitals in the second phase. It becomes the main focus in the third phase through computerized communication between departments, establishing big-data self-service machines, and standardized platforms. In the final phase, it expands to gathering information, hiring experts in data science, and contracting IT companies.
Table 6: Engineering characteristics for process control
| n | Engineering characteristics | Explanation |
| 1 | Gathering information | Collecting data and information in an appropriate way |
| 2 | Contracting consulting centers | Contracting specialist centers in data science, supply-chain management and anthropology |
| 3 | Facilitating payment methods | Making payment methods easier |
| 4 | Short breaks | Short breaks for physicians and other staff |
| 5 | Suitable areas for high-speed connection | Preparing a high-speed connection area for patients and staff |
| 6 | Contracting IT companies | Contracting a professional IT company |
| 7 | Instructions for using self-service machines | Placing instructions near self-service machines to help the users |
| 8 | Training quality department employees | Training employees in principles of quality and survey methods |
| 9 | Hiring experts in data sciences | Finding experts to analyze data |
| 10 | Government initiatives | Governmental initiatives, especially on standardized platforms |
| 11 | Incentives | Rewards to motivate and encourage employees |
5. Conclusion
KSA’s vision is to privatize public hospitals as part of its aim to improve the Saudi economy and make KSA one of the most competitive countries in the world [31]. This implies an increase in the demand for private healthcare services. Thus, tools for the assessment and development of quality need to be implemented. As shown in this study, QFD can be an effective and realistic tool because it considers the VOC. Utilizing QFD, it was found that information recording and flow have the greatest impact on improving service quality in healthcare. Scheduling also plays an important role in improving customer satisfaction, as it was given the greatest weight of all the engineering characteristics that have a strong correlation with customer requirements.
6. Future research
To develop a comprehensive QFD, all departments and expertise from different fields should be integrated, which would improve research in the field of healthcare service. Moreover, including the third factor of Donabadian’s model (outcomes) and considering it as a customer requirement may improve the implementation of the QFD in healthcare. Future research should focus on other stakeholders, such as nurses and physicians. Communication has a potential for further studies, which should concentrate on all aspects of communication, such as electronic communication and face-to-face interaction. Such studies would need to examine, evaluate, and enhance communication to achieve the standard requirements.
- R. Sajjad, M.O. Qureshi, “An assessment of the healthcare services in the Kingdom of Saudi Arabia: An analysis of the old, current, and future systems,” International Journal of Healthcare Management, 13(S1), 109–117, 2020, doi:10.1080/20479700.2018.1433459.
- M. Aljuaid, F. Mannan, Z. Chaudhry, S. Rawaf, A. Majeed, “Quality of care in university hospitals in Saudi Arabia: A systematic review,” BMJ Open, 6(2), 2016, doi:10.1136/bmjopen-2015-008988.
- C. Chow-Chua, M. Goh, “Quality improvement in the healthcare industry: Some evidence from Singapore,” International Journal of Health Care Quality Assurance, 13(5), 223–229, 2000, doi:10.1108/09526860010342725.
- D.A. Garvin, “What Does ‘Product Quality’ Really Mean?,” Sloan Management Review, 26(1), 25–43, 1984.
- M. Kanan, “Assessment of the COPQ due to poor maintenance practices in Saudi industry,” SSRG International Journal of Engineering Trends and Technology, 68(11), 163–172, 2020, doi:10.14445/22315381/IJETT-V68I11P222.
- A. Parasuraman, V.A. Zeithaml, L.L. Berry, “A Conceptual Model of Service Quality and Its Implications for Future Research,” Journal of Marketing, 49(4), 41, 1985, doi:10.2307/1251430.
- M. Dilber, N. Bayyurt, S. Zaim, M. Tarim, “Critical factors of total quality management and its effect on performance in health care industry: A Turkish experience,” Problems and Perspectives in Management, 3(4), 220–234, 2005.
- I.E. Chaniotakis, C. Lymperopoulos, “Service quality effect on satisfaction and word of mouth in the health care industry,” Managing Service Quality, 19(2), 229–242, 2009, doi:10.1108/09604520910943206.
- P. Padma, C. Rajendran, L.P. Sai, “A conceptual framework of service quality in healthcare: Perspectives of Indian patients and their attendants,” Benchmarking: An International Journal, 16(2), 157–191, 2009, doi:10.1108/14635770910948213.
- M.W. Usrey, K.J. Dooley, “T HE D IMENSIONS OF S O F T WA R E Q UA L I T Y.”
- J. Juran, Juran’s quality handbook, 2008, doi:10.1007/978-3-540-78773-0_5.
- I. Sila, M. Ebrahimpour, “Examination and comparison of the critical factors of total quality management (TQM) across countries,” International Journal of Production Research, 41(2), 235–268, 2003, doi:10.1080/0020754021000022212.
- G.J. Hahn, N. Doganaksoy, R. Hoerl, “The evolution of six sigma,” Quality Engineering, 12(3), 317–326, 2000, doi:10.1080/08982110008962595.
- S.M. Campbell, M.O. Roland, S.A. Buetow, “Defining quality of care,” Social Science and Medicine, 51(11), 1611–1625, 2000, doi:10.1016/S0277-9536(00)00057-5.
- D. Singh, K. Dixit, “Measuring Perceived Service Quality in Healthcare Setting in Developing Countries: A Review for Enhancing Managerial Decision-making,” Journal of Health Management, 22(3), 472–489, 2020, doi:10.1177/0972063420963407.
- C. Bergerum, A.K. Engström, J. Thor, M. Wolmesjö, “Patient involvement in quality improvement – a ‘tug of war’ or a dialogue in a learning process to improve healthcare?,” BMC Health Services Research, 20(1), 1–13, 2020, doi:10.1186/s12913-020-05970-4.
- A. Al Kuwaiti, F.A. Al Muhanna, “Challenges facing healthcare leadership in attaining accreditation of teaching hospitals,” Leadership in Health Services, 32(2), 170–181, 2019, doi:10.1108/LHS-01-2018-0002.
- NATIONAL.
- B. Canniff, “Public Health Accreditation: History, Implications, and Opportunities for Tribal Public Health,” Journal of Public Health Management and Practice, 24(3), S58–S59, 2018, doi:10.1097/PHH.0000000000000762.
- M.M. Siqueira, A.M. Malik, “Claudia A. S. Araujo (corresponding author) – Coppead Graduate School of Business, Federal University of Rio de Janeiro-RJ, Brazil. -,” 2020.
- M.M. Butt, E.C. de Run, “Private healthcare quality: Applying a SERVQUAL model,” International Journal of Health Care Quality Assurance, 23(7), 658–673, 2010, doi:10.1108/09526861011071580.
- M.J. Taylor, C. McNicholas, C. Nicolay, A. Darzi, D. Bell, J.E. Reed, “Systematic review of the application of the plan-do-study-act method to improve quality in healthcare,” BMJ Quality and Safety, 23(4), 290–298, 2014, doi:10.1136/bmjqs-2013-001862.
- J.R. Sharma, A.M. Rawani, M. Barahate, “Quality function deployment: a comprehensive literature review,” International Journal of Data Analysis Techniques and Strategies, 1(1), 78–103, 2008, doi:10.1504/IJDATS.2008.020024.
- L.K. Chan, M.L. Wu, Quality function deployment: A literature review, 2002, doi:10.1016/S0377-2217(02)00178-9.
- J.R. Hauser, D. Clausings, “The house of quality,” IEEE Engineering Management Review, 24(1), 24–32, 1996.
- B. Dehe, D. Bamford, “Quality Function Deployment and operational design decisions–a healthcare infrastructure development case study,” Production Planning and Control, 28(14), 1177–1192, 2017, doi:10.1080/09537287.2017.1350767.
- E.S. Jaiswal, “A Case Study on Quality Function Deployment (QFD),” IOSR Journal of Mechanical and Civil Engineering, 3(6), 27–35, 2012, doi:10.9790/1684-0362735.
- N.F.O. Sivaloganathan, S. and Evbuomwan, “CONCURRENT ENGINEERING: Research and Applications Quality State of the Art and Future Directions,” 5(2), 171–181, 1997.
- A. Al Memari, “Improving Healthcare Services by Quality Function Deployment (QFD) (QFD),” (2014148132), 2016.
- Y. Abdelsamad, M. Rushdi, B. Tawfik, “Functional and Spatial Design of Emergency Departments Using Quality Function Deployment,” Journal of Healthcare Engineering, 2018, 2018, doi:10.1155/2018/9281396.
- M.K. Al-Hanawi, A.M.N. Qattan, “An Analysis of Public-Private Partnerships and Sustainable Health Care Provision in the Kingdom of Saudi Arabia,” Health Services Insights, 12, 2019, doi:10.1177/1178632919859008.
- C.S. Dewa, D. Loong, S. Bonato, L. Trojanowski, “The relationship between physician burnout and quality of healthcare in terms of safety and acceptability: A systematic review,” BMJ Open, 7(6), 2017, doi:10.1136/bmjopen-2016-015141.
- C.P. Hunt, Robert A; Killen, Best practice quality function deployment (QFD) Part I: Cases, 117, Bradford: Emerald, 2004.