The Effects of Transmission Power and Modulation Schemes on the Performance of WBANs in on-Body Medical Applications
Volume 5, Issue 4, Page No 783–794, 2020
Adv. Sci. Technol. Eng. Syst. J. 5(4), 783–794 (2020);
 DOI: 10.25046/aj050493
DOI: 10.25046/aj050493
Keywords: Wireless Body Area Networks, IEEE 802.15.6, On-body medical applications, Packet Loss Rate, Throughput, Latency
Wireless Body Area Networks support the operation within multiple frequency bands. Thus, they can be integrated in several applications, one of which is on-body medical monitoring applications, as concerned in this paper. Therefore, the purpose of this study is to present the impact of transmission power and both of Differential Binary Phase Shift Keying and Differential Quadrature Phase Shift Keying modulation schemes, on the performance of a WBAN model based on the IEEE 802.15.6 2.4 GHz narrow-band, dedicated to on-body medical applications. This involves identifying the modulation scheme(s) and transmission power level(s) to be adopted for these applications, that can be classified into three types depending on their data rate (low, medium and high data rate medical applications), in order to meet Packet Loss Rate and latency requirements. The numerical study has confirmed that the adoption of DBPSK modulation and low transmission powers provides good performance for low data rate monitoring applications. At medium data rates, a relatively increased transmit power was required. However, at high data rates, DQPSK modulation with a 0 dBm transmission power seemed to be the right choice to be made in terms of the mentioned performance indicators.
1. Introduction
Brain tumors are tumor types located in the brain. The mortality rate is high. There are two different types: benign and malignant. Benign brain tumors, which have a slow growth rate, are easily separable from brain tissue. Malignant brain tumors grow faster and can damage nearby brain tissue[1]. There have been many successful studies in which computer were used in medical applications in recent years. Skin cancer [2], breast cancer [3], thyroid nodules [4] are some of these studies.
In addition, tumors originating from brain tissue are called primary brain tumors, while tumors formed by the splashing of cancerous cells that appear elsewhere in the body are called secondary brain tumors. The most common (65%) and most malignant brain tumor is glioblastoma [5]. Glioblastoma multiforme (GBM) is one of the deadliest cancer types and is a common type of malignant glioma in the central nervous system. With the development of computed tomography and magnetic resonance imaging (MRI), it has become increasingly clear that gliomas may have a multifocal or multicentric [6]. Although the diagnosis of multiple lesions becomes easier with the introduction of computed tomography into the field, the differential diagnosis of multiple cerebral lesions still remains a problem. In multifocal lesions, the lesions are localized in more than one part of the brain and there is a macroscopic or microscopic level relationship between them. In multicentric gliomas, there is neither macroscopic nor microscopic level relationship between lesions. The propagation path of multicentric lesions is unclear, but this situation is slightly different in multiple lesions. Multiple lesions create multiple cerebral areas using a systematic propagation pathway [7]. The correct detection of this condition is very important in the treatment of the disease.
Early diagnosis of brain tumors can change the course of the disease and save lives. On the other hand, computers perform complex operations in a very short time. Computers are used in many areas of life, especially in health, as it produces automatic, fast and accurate results. For this reason, computer-aided diagnostic (CAD) systems are frequently used today. CAD systems analyze the complex relationships in medical data and assist the doctor in decision making [8]. Salvati divided multifocal gliomas into four different categories. These are diffuse, multicentric, multiple and multi-organ. In addition, in his study, he divided his patients into multicentric and multifocal tumor groups and found that there was no significant difference between patients [9]. In a spike case, as malignant glial tumors damage nerve cells, it seems possible that the multicentricity of gliomas may also accompany multiple sclerosis [10]. DNN can learn quickly, automatically identify features, and can be successfully applied in computer learning systems. Besides that, DNNs are also used in some medical image analysis. It can be preferred especially in brain tumor segmentation and classification. It is designed the DNN model to segment brain separate gray and white matter from cerebrospinal fluid and analyzed the segmentation accuracy with DNN [11]. Similarly DNN model for the segmentation of brain tumors is proposed [12].
In this study, Deep Neural Network (DNN) architecture was proposed to classify the MR brain image features as n/a, multifocal, multicentric and gliomatosis. Synthetic Minority Over-sampling Technique (SMOTE) was used as a pre-processing. It has been determined that the pre-processing has a significant effect on the classification success.
2. Material and Methods
2.1. Dataset
In the study, The Repository of Molecular Brain Neoplasia Data (REMBRANDT) dataset [13] was used. The REMBRANDT dataset is a dataset of The Cancer Imaging Archive (TCIA) database shared by the National Cancer Institute. TCIA is an accessible archive containing medical images [14]. This data set contains images of 33 patients. Each patient has an average of 20 MR images, on separate axial, sagittal and coronal planes. For each patient, there are feature key values provided by 3 different neuroradiologists from Thomas Jefferson University (TJU) Hospital. This feature set is called VASARI (Visually Accessible Rembrandt Images). VASARI dataset was used in the classification process.
2.2. SMOTE
SMOTE is a method used in unbalanced data. Every minority class sample is taken and synthetic samples are created by looking at any or the sample’s entire k neighbour. Thus, the minority class is over-sampled [15]. The main difference from other sampling methods is the production of synthetic samples by looking at their neighbours, instead of copying and reproducing the minority class samples. Thus, it realizes class distribution without providing additional information.
2.3. Deep Neural Networks (DNN)
Machine learning technologies potentiate many technologies in the modern world. People use these technologies in many areas such as webcams, e-commerce activities, and mobile devices. In addition, it offers good results in complex problems. These are identifying objects from images, converting speech to text and matching web contents with the interests of the users. Traditional ML techniques have some limitations in processing raw data. Extracting features representing data in the raw form and converting them into feature vectors used as input for classifier is a difficult process that requires expertise [16].
Deep learning allows abstract representation of data by creating simple but nonlinear modules. In this way, it is possible to learn very complex functions. This structure reveals the distinguishing features between classes for classification problems. Deep learning produces successful results for many problems that cause problems in the advancement of artificial intelligence methods. It is used in many areas such as image recognition [17-19], speech processing [20, 21], and gene mutation prediction [22]. It is thought that DNN will make faster progress thanks to the new neural network structures proposed with an increase in computation capacity and amount of data [16].
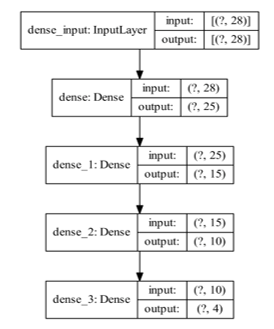
Deep neural network structure is shown in Figure 1.
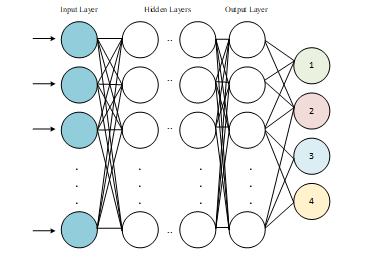 Figure 1: Deep Neural Network Schema [16]
Figure 1: Deep Neural Network Schema [16]
The development of computer hardware structure and the widespread use of GPU architecture facilitates and speed up the training of the complex and multi-layered neural networks as shown in Figure 1. In this way, more outstanding [23].
The mathematical model used in the neural network training stage is shown in Eq-1.
![]() According to Equation, represents the weight matrix in the nth layer and is activation function. This structure gives better results than single-layer networks [24].
According to Equation, represents the weight matrix in the nth layer and is activation function. This structure gives better results than single-layer networks [24].
In this study, a deep neural network design with 1 input, 1 output and 2 hidden layer was designed.
The increasing of software technologies shaped under three specialized topics such as artificial intelligence, machine learning and deep learning has caused an increase in interest in these three subjects. Deep Neural Networks finds the relationship between a range of inputs and outputs. Successful results in many areas such as image processing, natural language processing, voice recognition [25].
3. Results
The application was carried out on the open source Python program. Tensorflow and Keras libraries were used. The count plot of the data to be classified into classes is given in Figure 2.
All images included in the Rembrandt data set consist of axial, sagittal and coronal image planes with an average of 20 images per plane for a total of 33 patients. In the data set, 30 different features were obtained from each tumor brain MR image. Rembrandt images (VASARI) were analyzed by three TJU radiologists and features of the images were extracted. In this way, a data set
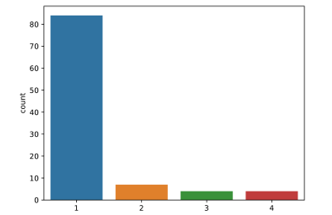 Figure 2: Count plot of data before SMOTE
Figure 2: Count plot of data before SMOTE
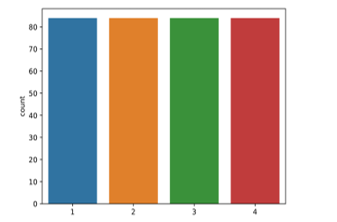 Figure 3: Count plot of data after SMOTE
Figure 3: Count plot of data after SMOTE
consisting of 99 patients and 30 different characteristic features used in the study. The data were classified according to n/a, multifocal, multicentric and gliomatosis. The data appears to be unbalanced. (84 n/a patient, 7 multifocal patient, 4 multicentric patient and 4 gliomatosis patient). For this reason, SMOTE pre-treatment was applied. Figure 3 shows the count plot after the SMOTE pre-processing.
The proposed DNN model is given in Figure 4. There are 3 hidden layers in the model, having 25, 15, and 10 filters, respectively. Model includes 1319 trainable parameters.
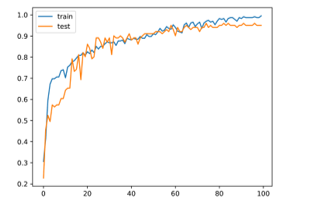
The activation function used in hidden layers is ReLu. The activation function used in the output layer is SoftMax. The optimizer who used the error back propagation phase is Adam. In this study, the data set was formed as 70% training and 30% test group. Figure 5 shows the change in accuracy on training and test data over 100 epochs.
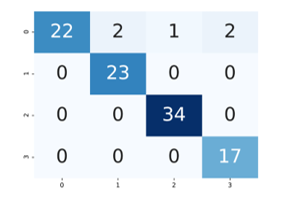
As can be seen from the graphic, the proposed method has overcome the over-fitting problem. Figure 6 shows confusion matrix.
DNN model was used to categorize brain tumors into four classes (n / a, multifocal, multicentric and gliomatosis). Four basic measurement indicators were used when evaluating the classification results. The proposed DNN classifier knew the opinion of radiologists with 95% accuracy. The success rate of the model was also examined with other performance metrics such as precision recall and F1. Respectively Precision, Recall, F1-measure values are 0.954, 0.950 and 0.949.
4. Discussion
Deep learning methods are used in many research fields of medical image analysis, from image recording, radiomic feature selection, segmentation and classification. Estimating the type of brain tumors is quite difficult and troublesome in the medical field.The aim of this study is to classify MR images of brain tumors as n/a, multifocal, multicentric and gliomatosis. In this study, unlike other studies, multiple cerebral lesions were classified. These lesions can have similar features and are difficult to classify. Studies in the literature determine tumor levels or predict whether the tumor is benign or malignant. Kumar and Vijay Kumar classified brain images as tumors and non-tumors using the Feed Forwarded Artificial neural network-based classifier and reached 91.17% accuracy with the ensemble classifier [26]. Glioblastoma and low-grade gliomas using logistic regression algorithm is classified with 0.88 accuracy [27]. Mahajani classified the MRI brain image as normal or abnormal with Back Propagation Neural Network (BPNN) and K Nearest Neighbor (KNN) algorithms. 70% accuracy using the KNN classifier and 72.5% accuracy using the BPNN classifier [28]. In the literature this dataset was tested with KNN, Random Forest (RF), Support Vector Machines (SVM), Linear Discriminant Analysis (LDA) machine learning algorithms. SVM algorithm with 90% accuracy rate was found to be better compared to other algorithms [29]. As seen in the examples, machine learning algorithms are commonly used approaches in classification. However, since deep learning models can analyze complex relationships effectively, it has gained an important place in machine learning in recent years. In another study, VGG-19 architecture used to classify brain tumors grades (I, II, III and IV) and achieve 0.90 accuracy and 0.96 average precision [30]. Also, in the other study it is classified the grades of glioma tumor using Convolutional Neural Networks (CNN) with an accuracy of 91.16% [31]. Compared to other algorithms, it has been seen that the applied method has advantages over traditional classifier algorithms. The complexity of the brain structure in the analysis of the brain image and the lack of imaging standards prevent the correct application of computer-aided learning systems in classifying brain tumors. Therefore, radiologist views come to the fore in determining these criteria. Table 1 shows some deep learning studies in the literature.
Table 1: Deep learning approaches for brain tumor classification
| Aim and Method | Accuracy |
| Tumor Segmentation-DNN[32] | 0.88 |
| Brain Tumour, CNN[33] | 91.43 |
| Brain Tumour, Capsule Network[34] | 86.56 |
| Brain Tumoru, DNN[35] | 90.66 |
In addition, proposed classification model can be tested with different parameters and radiomic features. Obtaining the data by experienced radiologists and determining the radiologist views with high accuracy is an indicator of the success of the algorithm. The Deep Learning approach facilitates researchers and trains the model using its own hyper parameters without specifying many features beforehand. But it is very important to apply the correct parameters to the model. In this study, the deep learning model was used and high accuracy was obtained with the correct parameters applied.
5. Conclusion
In the article, multifocal, multicentric and gliomatosis classification of brain tumors with SMOTE pre-processing of the DNN model were examined. The results show that the proposed method is very successful. The proposed method gives automatic, fast and accurate results. It can give an idea as a second look when doctors are unstable.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgment
No funding,
- S. Movassaghi, M. Abolhasan, J. Lipman, D. Smith and A. Jamalipour, “Wireless Body Area Networks: A Survey” IEEE Commun. Surv. Tut., 16(3), 1658-1686, 2014. https://doi.org /10.1109/SURV.2013.121313.00064.
- A. Es-saqy, M. Abata, S. Mazer, M. Fattah, M. Mehdi, M. El bekkali and C. Algani, “Very Low Phase Noise Voltage Controlled Oscillator for 5G mm-wave Communication Systems” in 2020 1st International Conference on Innovative Research in Applied Science, Engineering and Technology (IRASET), Meknes, Morocco, 2020. https://doi.org /10.1109/IRASET48871.2020.9092005.
- S. Ullah, “A Review of Wireless Body Area Networks for Medical Applications” Int’l J. Commun. Netw. Syst. Sci., 02(08), 797–803, 2009. https://doi.org /10.4236/ijcns.2009.28093.
- Boulemtafes A., Badache N. “Design of Wearable Health Monitoring Systems: An Overview of Techniques and Technologies” mHealth Ecosystems and Social Networks in Healthcare. Springer, Chamv, 2016.
- R. Negra, I. Jemili, and A. Belghith, “Wireless Body Area Networks: Applications and Technologies” Procedia Comput. Sci., 83, 1274–1281, 2016. https://doi.org /10.1016/j.procs.2016.04.266.
- B. Antonescu and S. Basagni, “Wireless body area networks: Challenges, trends and emerging technologies” in BODYNETS 2013 – 8th Int. Conf. Body Area Networks, 2013. https://doi.org /10.4108/icst.bodynets.2013.253722.
- M. Boumaiz, M. El ghazi, S. Mazer, M. Fattah, A. Bouayad, M. El bekkali, and Y. Balboul, “Energy harvesting based WBANs: EH optimization methods” Procedia Comput. Sci., 151, 1040–1045, 2019. https://doi.org /10.1016/j.procs.2019.04.147.
- Z. Jin, J. Oresko, S. Huang, and A. C. Cheng, “HeartToGo: A personalized medicine technology for cardiovascular disease prevention and detection” in 2009 IEEE/NIH Life Science Systems and Applications Workshop, Bethesda, MD, 2009. https://doi.org /10.1109/LISSA.2009.4906714.
- M. Hadjem, O. Salem and F. Naït-Abdesselam, “An ECG monitoring system for prediction of cardiac anomalies using WBAN” in 2014 IEEE 16th International Conference on e-Health Networking, Applications and Services (Healthcom), Natal, 2014. https://doi.org /10.1109/HealthCom.2014.7001883.
- Ullah, S., Higgins, H., Braem, B. Latre, B. Blondia, C. Moerman, I. Saleem, S. Rahman, Z. and Kwak, K, S. “A Comprehensive Survey of Wireless Body Area Networks”. J Med Syst. 36(3), 1065-1094. https://doi.org /10.1007/s10916-010-9571-3.
- Huzooree G., Khedo K.K., Joonas N. “Wireless Body Area Network System Architecture for Real-Time Diabetes Monitoring” In: Fleming P., Vyas N., Sanei S., Deb K. Emerging Trends in Electrical, Electronic and Communications Engineering. Springer, Cham, 2016.
- M. Udin Harun Al Rasyid, F. A. Saputra, and A. Christian, “Implementation of blood glucose levels monitoring system based on Wireless Body Area Network” in 2016 IEEE Int. Conf. Consum. Electron, 2016. https://doi.org /10.1109/ICCE-TW.2016.7521005.
- Hsueh-Ting Chu, Chir-Chang Huang, Zhi-Hui Lian and J. J. P. Tsai, “A ubiquitous warning system for asthma-inducement” in IEEE International Conference on Sensor Networks, Ubiquitous, and Trustworthy Computing (SUTC’06), Taichung, 2006. https://doi.org /10.1109/SUTC.2006.20.
- K. Revett and S. T. De Magalhães, Cognitive biometrics: Challenges for the future, Springer, Berlin, Heidelberg, 2010.
- T. M. Connolly, E. A. Boyle, E. Macarthur, T. Hainey, and J. M. Boyle, “Computers & Education A systematic literature review of empirical evidence on computer games and serious games” Comput. Educ., 59(2), 661–686, 2012. https://doi.org /10.1016/j.compedu.2012.03.004.
- K. Hasan, K. Biswas, K. Ahmed, N. S. Nafi, and M. S. Islam, “A comprehensive review of wireless body area network” J. Netw. Comput. Appl., 143, 178–198, 2019. https://doi.org /10.1016/j.jnca.2019.06.016.
- R. Cavallari, F. Martelli, R. Rosini, C. Buratti, and R. Verdone, “A survey on wireless body area networks: Technologies and design challenges” IEEE Commun. Surv. Tutorials, 16(3), 1635–1657, 2014. https://doi.org / 10.1109/SURV.2014.012214.00007.
- P. Mathew, L. Augustine, D. Kushwaha, D. Vivian and D. Selvakumar, “Hardware implementation of NB PHY baseband transceiver for IEEE 802.15.6 WBAN” in 2014 International Conference on Medical Imaging, m-Health and Emerging Communication Systems (MedCom), Greater Noida, 2014. https://doi.org /10.1109/MedCom.2014.7005977.
- Wang, Y., & Wang, Q. “Evaluating the IEEE 802.15.6 2.4GHz WBAN Proposal on Medical Multi-Parameter Monitoring under WiFi/Bluetooth Interference” International Journal of E-Health and Medical Communications (IJEHMC), 2(3), 48-62, 2020. https://doi.org /10.4018/jehmc.2011070103 103.
- IEEE Standard for Local and metropolitan area networks – Part 15.6: Wireless Body Area Networks,” in IEEE Std 802.15.6-2012, 1-271, 2012. https://doi.org /10.1109/IEEESTD.2012.6161600.
- S. AhmadSalehi, , M.A Razzaque, I. Tomeo-Reyes and N. Hussain, “IEEE 802.15.6 standard in wireless body area networks from a healthcare point of view” in 2016 22nd Asia-Pacific Conference on Communications (APCC), 2016. https://doi.org /10.1109/APCC.2016.7581523.
- M. Boumaiz, M. E. Bekkali, A. Bouayad and M. Fattah, “The Impact of Distance between Neighboring WBANs on IEEE 802.15.6 Performances” in 2019 7th Mediterranean Congress of Telecommunications (CMT), Fès, Morocco, 2019. https://doi.org /10.1109/CMT.2019.8931341.
- M. Boumaiz, M. El Ghazi, M. Fattah, A. Bouayad, and M. El Bekkali, “Mutual coexistence in WBANs: Impact of modulation schemes of the IEEE 802.15.6 standard” Int. J. Adv. Comput. Sci. Appl., 11(5), 294–302, 2020. https://doi.org /10.14569/IJACSA.2020.0110539.
- M. Boumaiz, M. El ghazi, A. Bouayad, M. Fattah, M. El bekkali and S. Mazer, “The impact of transmission power on the performance of a WBAN prone to mutual interference” in 2019 International Conference on Systems of Collaboration Big Data, Internet of Things & Security (SysCoBIoTS), Casablanca, Morocco, 2019. https://doi.org /10.1109/SysCoBIoTS48768.2019.9028035.
- F. Di Franco, C. Tachtatzis, R. C. Atkinson, I. Tinnirello and I. A. Glover, “Channel estimation and transmit power control in wireless body area networks” in IET Wireless Sensor Systems, 5(1), 11-19, 2015. https://doi.org /10.1049/iet-wss.2013.0070.
- K. Takizawa, A. Aoyagi, J. Takada, N. Katayama, K. Yekeh, Y. Takehiko and K. Kohno. “Channel models for wireless body area networks”, in 2008 30th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Vancouver, BC, 2008. https://doi.org /10.1109/IEMBS.2008.4649465
- M. Shu, D. Yuan, C. Zhang, Y. Wang, and C. Chen, “A MAC protocol for medical monitoring applications of wireless body area networks,” Sensors (Switzerland), 15(6), 12906–12931, 2015. https://doi.org /10.3390/s150612906.
- P. S. Hall, “Antennas Challenges for Body Centric Communications” in 2007 International workshop on Antenna Technology: Small and Smart Antennas Metamaterials and Applications, Cambridge, 2007. https://doi.org /10.1109/IWAT.2007.370076.
- S. L. Cotton, R. D’Errico, and C. Oestges, “A review of radio channel models for body centric communications”. Radio science, 49(6), 371–388, 2014. https://doi.org/10.1002/2013RS005319
- B. Hazarika, B. Basu, and J. Kumar, “A Multi-Layered Dual-Band On-Body Conformal Integrated Antenna for WBAN Communication” Aeu-int J Electron C., 95, 226-235, 2018. https://doi.org /10.1016/j.aeue.2018.08.021.
- I. Suriya and R. Anbazhagan, “Inverted-A based UWB MIMO antenna with triple-band notch and improved isolation for WBAN applications,” Aeu-int J Electron C., 99, 25–33, 2019. https://doi.org /10.1016/j.aeue.2018.11.030.
- K. Y. Yazdandoost, Channel Modeling Subcommittee Report. 2010.
- M. Boumaiz, M. El ghazi, S. Mazer, M. El bekkali, A. Bouayad and M. Fattah, “Performance analysis of DQPSK and DBPSK modulation schemes for a scheduled access phase based Wireless Body Area Network” in 2019 9th International Symposium on Signal, Image, Video and Communications (ISIVC), Rabat, Morocco, 2018. https://doi.org /10.1109/ISIVC.2018.8709232.
- A. Wong, M. Dawkins, G. Devita, N. Kasparidis, A. Katsiamis, O. King, F. Lauria, J. Schiff and A. Burdett., “A 1V 5mA multimode IEEE 802.15.6/bluetooth low-energy WBAN transceiver for biotelemetry applications” in IEEE International Solid-State Circuits Conference, San Francisco, CA, 2012. https://doi.org /10.1109/ISSCC.2012.6177022.
- F. Martelli, C. Buratti and R. Verdone, “On the performance of an IEEE 802.15.6 Wireless Body Area Network” in 17th European Wireless 2011 – Sustainable Wireless Technologies, Vienna, Austria, 2011.
- H. Zhang, F. Safaei, and L. C. Tran, “Joint transmission power control and relay cooperation for WBAN systems” Sensors (Switzerland), 18(12), 1–26, 2018. https://doi.org /10.3390/s18124283.
- L. Skorin-Kapov and M. Matijasevic, “Analysis of QoS requirements for e-Health services and mapping to evolved packet system QoS classes” Int. J. Telemed. Appl., 2010. https://doi.org /10.1155/2010/628086.
- D. Vouyioukas, I. Maglogiannis, and D. Komnakos, “Emergency m-Health Services through High-Speed 3G Systems: Simulation and Performance Evaluation” Simulation, 83(4), 329–345, 2007. https://doi.org /10.1177/0037549707083113.
- M. A. Yigitel, O. D. Incel, and C. Ersoy, “QoS-aware MAC protocols for wireless sensor networks: A survey,” Comput. Networks, 55(8), 1982–2004, 2011. https://doi.org /10.1016/j.comnet.2011.02.007.
- M. A. Razzaque, S. S. Javadi, Y. Coulibaly, and M. T. Hira, “Qos-aware error recovery in wireless body sensor networks using adaptive network coding,” Sensors (Switzerland), 15(1), 440–464, 2015. https://doi.org /10.3390/s150100440.
- A. Maroua and F. Mohammed, “Characterization of Ultra Wide Band indoor propagation”. in 2019 7th Mediterranean Congress of Telecommunications (CMT), Fès, Morocco, 2019. https://doi.org /10.1109 / CMT.2019.8931367.
- Vítor Viegas, J. M. Dias Pereira, Pedro Girão, Octavian Postolache, "Study of latencies in ThingSpeak", Advances in Science, Technology and Engineering Systems Journal, vol. 6, no. 1, pp. 342–348, 2021. doi: 10.25046/aj060139
- Lincan Li, Chiew Foong Kwong, Qianyu Liu, "A Proactive Mobile Edge Cache Policy Based on the Prediction by Partial Matching", Advances in Science, Technology and Engineering Systems Journal, vol. 5, no. 5, pp. 1154–1161, 2020. doi: 10.25046/aj0505140
- Rahardhita Widyatra Sudibyo, Nobuo Funabiki, Minoru Kuribayashi, Kwenga Ismael Munene, Md. Manowarul Islam, Wen-Chung Kao, "A Proposal of TCP Fairness Control Method for Two-Host Concurrent Communications in Elastic WLAN System Using Raspberry Pi Access-Point", Advances in Science, Technology and Engineering Systems Journal, vol. 4, no. 6, pp. 10–18, 2019. doi: 10.25046/aj040602
- Kwenga Ismael Munene, Nobuo Funabiki, Md. Manowarul Islam, Minoru Kuribayashi, Md. Selim Al Mamun, Wen-Chung Kao, "An Extension of Throughput Drop Estimation Model for Three-Link Concurrent Communications under Partially Overlapping Channels and Channel Bonding in IEEE 802.11n WLAN", Advances in Science, Technology and Engineering Systems Journal, vol. 4, no. 4, pp. 94–105, 2019. doi: 10.25046/aj040411
- Lev Lafayette, Bernd Wiebelt, Dirk von Suchdoletz, Helena Rasche, Michael Janczyk, Daniel Tosello, "The Chimera and the Cyborg", Advances in Science, Technology and Engineering Systems Journal, vol. 4, no. 2, pp. 1–7, 2019. doi: 10.25046/aj040201
- Zifan Zhou, Michael Stübert Berger, Sarah Renée Ruepp, Ying Yan, "Insight into the IEEE 802.1 Qcr Asynchronous Traffic Shaping in Time Sensitive Network", Advances in Science, Technology and Engineering Systems Journal, vol. 4, no. 1, pp. 292–301, 2019. doi: 10.25046/aj040128
- Havva Esra Bilisik, Radosveta Sokullu, "A Novel Fair and Efficient Resource Allocation Scheduling Algorithm for Uplink in LTE-A", Advances in Science, Technology and Engineering Systems Journal, vol. 3, no. 6, pp. 222–232, 2018. doi: 10.25046/aj030629
- Akbor Aziz Susom, "Effectiveness of Routing Protocols for Different Networking Scenarios", Advances in Science, Technology and Engineering Systems Journal, vol. 3, no. 4, pp. 112–121, 2018. doi: 10.25046/aj030412